Abstract
The genomic landscape of myeloproliferative neoplasms (MPNs) has altered dramatically due to the recent discovery of somatic mutations of calreticulin (CALR). This discovery enables for the first time molecular information, in addition to JAK2V617F, to be used in the majority of MPN patients as an affirmative variable to discriminate MPNs from reactive myeloid proliferations. The clinical course of essential thrombocythemia (ET) or primary myelofibrosis (PMF) in patients carrying the CALR mutation was reported to be more indolent than in JAK2 positive patients and was associated with increased survival. Our aim was to investigate whether the impact of CALR expression on prognosis and clinical outcome is different in prefibrotic/early PMF (prePMF) compared to WHO-ET.
In a cohort of 348 adult patients with the clinical diagnosis of either ET or PMF mutational analysis for CALR was available. Eligibility criteria for the study included: availability of mutation analysis for JAK2, MPL and CALR; availability of representative, treatment-naive bone marrow biopsy (BM); availability of a histological and clinical consensus on the diagnosis; complete long-term documentation of clinical data and outcome.
Consenting clinico-pathological findings in our cohort were consistent with 115 cases showing WHO-ET and 85 patients with prePMF. In comparison to WHO-ET, prePMF revealed minor/borderline age- and gender-matched anemia, slight increase in serum LDH level and leukocyte count, minor to slight splenomegaly, and an occasional left shift in granulo- and erythropoiesis with occurrence of a few myelo-and/or erythroblasts (table 1). An accurate differentiation between both MPN entities was shown to exert a significant difference in terms of overall and relative survival and hematologic transformation into overt PMF and AL. The present study revealed a different CALR mutation frequency in ET in contrast to most of the investigations published recently. We observed CALR mutations in 18% of WHO-ET; JAK2, MPL and CALR wildtype (wt) was observed in 13% of WHO-ET. The discrepancy in the frequencies of CALR positivity in our ET cohort to most of the recently published studies may be due to our strict adherence to the WHO criteria for diagnosis of ET. Regarding prePMF, we observed CALR mutations in 39% of the patients. 92% of the JAK2 and MPL wt subgroup carried the CALR mutation, with JAK2, MPL and CALR wt being observed in only 3% of prePMF.
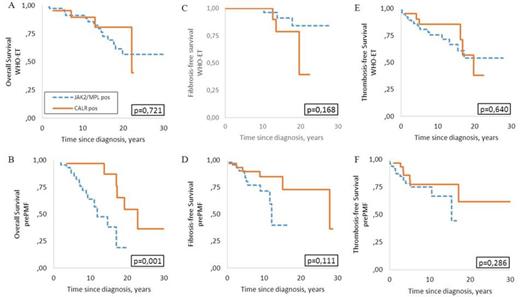
The most remarkable differences between WHO-ET and prePMF were seen in the comparison of the overall survival (figure 1). While the CALR mutation did not have any beneficial influence on survival in WHO-ET, it was associated with a superior overall survival in prePMF. Such a striking difference was not seen at the time of transformation into overt myelofibrosis, and there was only a slightly shorter time to progression to fibrosis in CALR wt prePMFs. There was a trend showing that CALR mutated prePMF patients have shorter thrombosis-free survival compared to CALR wt prePMF patients. There was no impact of the CALR mutations on thrombosis-free survival in WHO-ET.
The present data confirm that WHO-ET and prePMF are biologically different sub-entities of MPNs. In prePMF, almost 100% of patients are now associated with a known disease-causing mutation. Our data support the classical clinical approach in the diagnosis of thrombocytosis, using BM histology to differentiate WHO-ET from prePMF and to estimate the outcome of the disease more accurately.
| . | Total cohort (N=200) . | WHO-ET (N=115) . | prePMF (N=85) . | P . |
|---|---|---|---|---|
| Age at diagnosis, years | 0,04 | |||
| median | 58,85 | 56,4 | 60,7 | |
| range | 19-88 | 19-84 | 27-88 | |
| Sex | 0,587 | |||
| male | 78 | 43 | 35 | |
| female | 122 | 72 | 50 | |
| Hb, g/dL | <0,001 | |||
| median | 14,1 | 14,3 | 13,5 | |
| range | 8,1-17,6 | 8,8-17,6 | 8,1-16,6 | |
| WBC, x109/l | 0,054 | |||
| median | 9,25 | 8,99 | 9,6 | |
| range | 4,01-24,54 | 4,92-22,3 | 4,01-24,54 | |
| Platelets, x109/l | 0,739 | |||
| median | 770 | 770 | 794 | |
| range | 78-2530 | 414-2490 | 78-2530 | |
| Palpable splenomegaly | <0,001 | |||
| No. | 51 (12 unk, 1 splenectomy) | 16 (7 unk, 1 splenectomy) | 35 (5 unk) | |
| % | 25,5 | 13,9 | 41,2 | |
| Fibrotic transformations | <0,001 | |||
| No. | 24 (10 unk) | 6 (1 unk) | 18 (9 unk) | |
| % | 12 | 5,2 | 21,2 | |
| Thrombotic events | 0,439 | |||
| No. | 39 (1 unk) | 22 (1 unk) | 17 | |
| % | 19,5 | 19 | 20 | |
| prev thrombosis | 0,042 | |||
| No. | 50 | 34 | 16 | |
| % | 25 | 30,4 | 18,8 | |
| JAK2 V617F pos | 0,08 | |||
| No. | 120 | 75 | 45 | |
| % | 60 | 65,2 | 52,9 | |
| CALR pos | 0,001 | |||
| No. | 54 | 21 | 33 | |
| % | 27 | 18,3 | 38,8 | |
| MPL pos | 0,189 | |||
| No. | 8 | 4 | 4 | |
| % | 4 | 3,5 | 4,7 | |
| JAK2/MPL/CALR wt | 0,0029 | |||
| No. | 18 | 15 | 3 | |
| % | 9 | 13 | 3,5 |
| . | Total cohort (N=200) . | WHO-ET (N=115) . | prePMF (N=85) . | P . |
|---|---|---|---|---|
| Age at diagnosis, years | 0,04 | |||
| median | 58,85 | 56,4 | 60,7 | |
| range | 19-88 | 19-84 | 27-88 | |
| Sex | 0,587 | |||
| male | 78 | 43 | 35 | |
| female | 122 | 72 | 50 | |
| Hb, g/dL | <0,001 | |||
| median | 14,1 | 14,3 | 13,5 | |
| range | 8,1-17,6 | 8,8-17,6 | 8,1-16,6 | |
| WBC, x109/l | 0,054 | |||
| median | 9,25 | 8,99 | 9,6 | |
| range | 4,01-24,54 | 4,92-22,3 | 4,01-24,54 | |
| Platelets, x109/l | 0,739 | |||
| median | 770 | 770 | 794 | |
| range | 78-2530 | 414-2490 | 78-2530 | |
| Palpable splenomegaly | <0,001 | |||
| No. | 51 (12 unk, 1 splenectomy) | 16 (7 unk, 1 splenectomy) | 35 (5 unk) | |
| % | 25,5 | 13,9 | 41,2 | |
| Fibrotic transformations | <0,001 | |||
| No. | 24 (10 unk) | 6 (1 unk) | 18 (9 unk) | |
| % | 12 | 5,2 | 21,2 | |
| Thrombotic events | 0,439 | |||
| No. | 39 (1 unk) | 22 (1 unk) | 17 | |
| % | 19,5 | 19 | 20 | |
| prev thrombosis | 0,042 | |||
| No. | 50 | 34 | 16 | |
| % | 25 | 30,4 | 18,8 | |
| JAK2 V617F pos | 0,08 | |||
| No. | 120 | 75 | 45 | |
| % | 60 | 65,2 | 52,9 | |
| CALR pos | 0,001 | |||
| No. | 54 | 21 | 33 | |
| % | 27 | 18,3 | 38,8 | |
| MPL pos | 0,189 | |||
| No. | 8 | 4 | 4 | |
| % | 4 | 3,5 | 4,7 | |
| JAK2/MPL/CALR wt | 0,0029 | |||
| No. | 18 | 15 | 3 | |
| % | 9 | 13 | 3,5 |
Thiele:AOP Orphan Pharmaceuticals: Consultancy, Honoraria; Incyte Corporation: Consultancy, Honoraria; Novartis: Consultancy, Honoraria, Research Funding; Shire: Consultancy, Honoraria, Research Funding; Sanofi: Consultancy, Honoraria.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal