Abstract
Background: Second generation tyrosine kinase inhibitors (2G-TKIs) are more potent than imatinib against chronic myeloid leukemia in chronic phase (CML-CP) as a first-line therapy, and the majority of patients (pts) on 2G-TKIs could achieve favorable molecular responces over MR3.0 by 24 M (Saglio G, et al. Blood 2011, Kantarjian HM, et al. Blood 2012). It is also likey that molecular response at 3 M will predict outcome for CML-CP pts on imatinib. Furthermore, Mustjoki S, et al. showed that Ph+ stem cell burden at diagnosis is a prognostic marker of molecular responses at 3-9 M on dasatinib or imatinib (Leukemia 2013). Thus, early prognostic marker of outcome is feasible for CML-CP on TKIs.
Methods: We are conducting a phase II study (N-road) for newly diagnosed CML-CP pts, in which nilotinib 300mg BID is given for 24 M and is to be escalated to 400mg BID if no optimal response at any check points. The primary endpoint is CMR rate by 24 M, and secondary endpoints include MR3.0/MR4.0 by 12 M and exploring prognostic factors. In this setting, the impact of initial Ph+ stem cell burden on clinical findings and therapeutic responses has been investigated in a sub-study. By July 2014, 48 pts were enrolled and BM CD34+ cell fractions could be evaluated by FACS-FISH analysis at diagnosis in 43 pts, among those 35 pts passed 3 M, 34 pts 6 M and 15 pts 12 M, respectively.
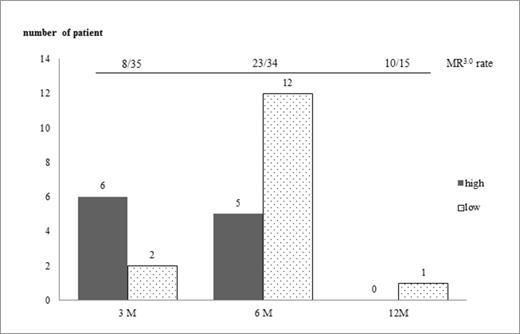
Results: MR3.0 rate was 8/35 at 3M, 23/34 at 6M and 10/15 at 12M. When 43 pts were classified into two groups (higher: H, lower: L) according to the mean CD34+ cell counts at diagnosis (5995/mL of BM aspirates), there were significant differences (p<0.05) in BCR-ABL transcripts indicated as IS (77.66 vs 64.03 %, p=0.030) and WBC count (81.3 vs 22.3 /mL, p=0.012), but no differences in molecular responses at 3, 6 and 12 M between the two groups. There was a positive correlation between CD34+ cell count and WBC count (r=0.328, p=0.035).
The median percentage of Ph+ cells, as measured by FISH (~1000 cells analyzed), in CD34+CD38- fraction at diagnosis was 97.1% (range 2-100%) compared to 98.6% (range 28.2-99.8%) in CD34+CD38+ fraction. The proportion of Ph+ cells in CD34+CD38- fraction correlated with PLT count (r=0.394, p=0.014) but inversely with RBC count (r=-0.474, p=0.003), Hb (r=-0.587, p=0.0001) and Ht (r=-0.475, p=0.003), respectively. Between the two groups divided by the median percentage, there were significant differences in RBC count (406 vs 460 x104/mL, p=0.046), Hb (11.7 vs 14.5 g/dL, p=0.009) and Hct (38.8 vs 44.7%, p=0.040). There were no significant differences in molecular responses at any check points. On the other hand, when divided by the mean percentage (81.1%), there was only a significant difference in PLT count (48.1 vs 27.2 /mL, p=0.028).
Absolute Ph+ cell counts in CD34+CD38- fraction were estimated in each patient by combining 3 parameters of CD34 cell counts/mL of BM aspirates, proportion of CD38- fraction and percentage of Ph+ cells. Ph+CD34+CD38- cell counts siginificantly correlated with WBC count (r=0.365, p=0.021) and inversely with RBC count (r=-0.361, p=0.002), Hb (r=-0.409, p=0.009) and percentage of lymphocytes (r=-0.339, p=0.032). Between the 2 groups divided by the median cell counts (256/mL), there were significant differences in RBC (406.5 vs 472.0 x104/mL, p=0.005), Hb (11.8 vs 14.3 g/dL, p=0.004), Hct (39.0 vs 44.6 %, p=0.024). Although we could not find significant difference in molecular responses at any check points, patients with lower number of Ph+CD34+CD38- cells tend to achieve MR3.0 faster than those with higher number of cells (p=0.059) (Figure 1). When divided by the mean cell counts (578/mL), there was a significant difference in WBC count (94.45 vs 22.44 /mL, p=0.016).
Conclusion: increased Ph+ stem cell burden apparently affects the level of leukocytosis and anemia at diagnosis, but not MR3.0/MR4.0 rate by 12 M on nilotinib, although it is likely to extend time to achieve MR3.0.
Nishiwaki:Novartis: Research Funding. Sugimoto:Novartis: Speakers Bureau. Shimizu:Novartis: Speakers Bureau. Wakita:Novartis: Speakers Bureau. Tojo:Novartis: Research Funding, Speakers Bureau.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal