Abstract
Background: Post transplant lymphoproliferative disorders (PTLD) are rare pathologically and clinically heterogeneous diseases arising in the setting of immunosuppression following hematopoietic stem cell and solid organ transplants (SOT). Our understanding of PTLD is restricted by its low incidence and heterogeneous treatment approaches, resulting in paucity of data. We sought to further describe characteristics and outcomes in PTLD patients who underwent treatment at our institution.
Methods and Patients: We performed a retrospective study to describe our institutional experience in a relatively large cohort of PTLD patients after SOT. Patient and disease characteristics were examined and prognostic factors for survival were determined using univariate and multivariate Cox analysis.
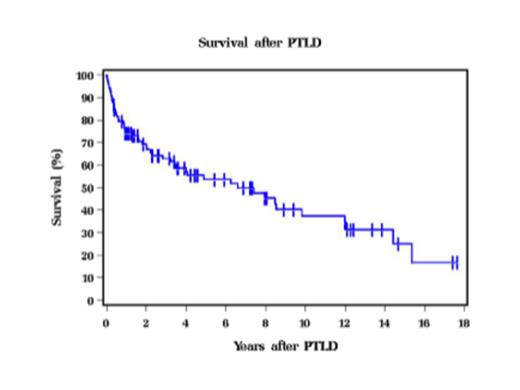
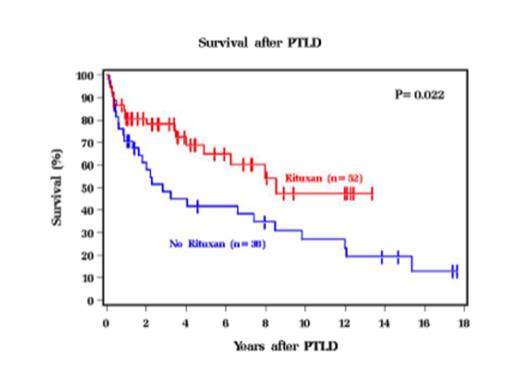
Results: Between May 1987 to January 2014, 98 patients with a confirmed diagnosis of PTLD underwent treatment at our institution. Median time from SOT to PTLD diagnosis was 60 months with median follow of 68 months from PTLD diagnosis. Baseline characteristics include male gender 77%, ECOG performance status (PS) 0-1 in 61%, and stage III-IV 69% with a median age at diagnosis of 47 years. Most common transplanted organ included heart 30%, lung 24%, kidney 20% and liver 19% and median time from SOT to PTLD diagnosis was 60 months. Most cases had monomorphic histology (81%) and were EBV+ (82%). Graft involvement and rejection were observed in 32% and 43% respectively. Of the 84% with extranodal (EN) involvement, gastrointestinal tract (37%) and lung (27%) were the common sites, while 3.2% had bone marrow (BM) involvement. Central nervous system (CNS) was involved in 11% of the cases. Only 58% received rituximab as part of the initial therapy, as significant part of our cohort was treated prior to rituximab era. Reduction in immunosuppression (73%), chemotherapy (40%), radiation (11%) and surgery (8%) were utilized either as single modality or in combination for treatment. Of the 66 patients with response data, 59% had complete response (CR) and 14% had progressive disease (PD). Relapse occurred in 23% of cases. Median overall survival (OS) from diagnosis of PTLD was 6 years (Figure 1), but in rituximab treated patients it was 8 years. On univariate analysis, higher age at diagnosis (HR 1.19, 95% CI 1.01-1.40, p=0.033), lung transplant (HR 2.42, 95% CI 1.36-4.33, p=0.003), higher IPI (HR 1.83, 95% CI 1.40-2.39, p=<0.001), decreased PS (HR 2.43, 95% CI 1.70-3.48, p=<0.001), and platelet count <200,000 (HR 2.84, 95% CI 1.27-6.33, p=0.011) were associated with lower OS, whereas liver transplant (HR 0.24, 95% CI 0.09-0.68, p=0.007) and GI involvement (HR 0.47, 95% CI 0.24-0.95, p=0.036) predicted better OS. Rituximab treatment (Figure 2) and achieving CR were associated with better OS. Histology, EN involvement, and EBV status were not significant predictors for survival. On multivariate analysis only lung transplant, IPI, and PS were predictive for OS. Lung transplant patients had a higher risk of mortality compared to other SOT (HR 2.63, 95% CI 1.39-4.95, p=0.003). Both higher IPI (HR 1.66, 95% CI 1.18-2.32, p=0.003) and poor PS (HR 1.94, 95% CI 1.27-2.96, p=0.002) were associated with inferior OS.
Conclusions: In this large cohort of PTLD patients after SOT, lung transplants, higher IPI and poor PS were identified as poor prognostic factors for OS on both univariate and multivariate analysis. Rituximab treatment was a favorable prognostic factor for OS that resulted in prolonged survival observed in this cohort.
Hill:Millenium: Research Funding; Novartis: Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal