Abstract
Background. Recent clinical trials based on immunotherapies targeting the PD-1/PD-L1 pathway have shown striking durable responses in a subset of patients with solid cancers. The Programmed death 1 (PD-1) protein is a key immune checkpoint inhibitor expressed by activated T cells. Its ligand, PD-L1, was reported highly expressed by tumor cells in some diffuse large B-cell lymphomas (DLBCL) of non-Germinal Center phenotype. We recently reported on the French multicenter GOELAMS075 trial that pre-treatment soluble PD-L1 (sPD-L1) in plasma was elevated in DLBCL patients compared to controls, and that elevated sPD-L1 was associated with inferior overall survival (OS), independent of the International Prognostic Index (IPI) and other clinical factors (Rossille et al., Leukemia 2014). Here, we replicate and extend these findings in two independent studies from Australia and the US.
Methods. The protein expression of sPD-L1 was evaluated using a commercial ELISA kit. The French discovery cohort consisted of 288 adults with newly diagnosed aggressive DLBCL, age 18 to 60 years, and treated with R-CHOP or high dose chemotherapy plus rituximab followed by autologous stem cell support (clinicaltrials.gov: NCT00561379); there were also 60 controls. The Australian study consisted of 51 DLBCL patients age 18 to 71 years, all stages, treated with R-CHOP14, along with 57 controls. The US study was an observational cohort from the Iowa/Mayo Lymphoma SPORE and consisted of 225 DLBCLs, age 19 to 92 years, all stages, treated with immunochemotherapy, along with 98 controls. Plasma samples were collected pre-treatment using EDTA tubes for the Australian and the US cohorts, BDª P100 tubes for the French cohort. sPD-L1 expression was measured in Rennes, France (French & US samples) and in Brisbane, Australia (Australian samples).The Kaplan-Meier method and Cox regression were used to model the association of sPD-L1 with OS. The 95th percentile of the sPD-L1 levels in each matched control group was used as the cutoff point to define elevated sPD-L1 levels.
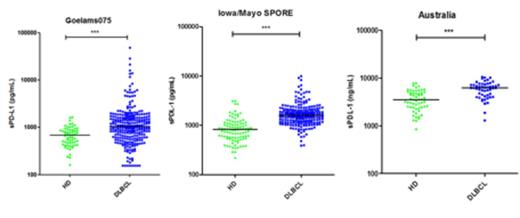
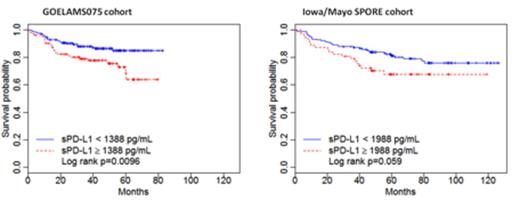
Results. Replicating the French findings, sPD-L1 levels were significantly higher for DLBCL patients compared to controls in both the US (P<0.0001) and Australian (P<0.0001) studies (Figure 1 ). The odds ratios for elevated sPD-L1 among patients compared to controls were 10.7 (95% CI 3.3-22.0), 8.9 (95% CI 3.1-25.3) and 12.6 (95% CI 2.7-28.0) for the French, US and Australian studies, respectively. In the French cohort, elevated sPD-L1 levels were associated with inferior OS (Hazard Ratio (HR)=2.05; 95% CI 1.18-3.57), and this was replicated in the US cohort (HR=1.71; 95% CI 0.97-3.01) (Figure 2 ). Due to the similarity of the results, we next pooled the French and US cohorts to increase power for multivariate and subset analyses. The median age at diagnosis of the 513 patients was 54 years; 29% were more than 60 years old; 69% of the patients had stage III-IV disease; 56% were IPI intermediate-risk and 9% were IPI high-risk patients. The median follow-up was 48 months (range, 0.5-126) overall, and 66 months for the patients still alive; there were 102 deaths. Using a cutpoint of 1729 pg/mL from the combined studies, patients with elevated sPD-L1 had inferior OS compared to patients without elevated sPD-L1, with 3-year OS rates estimated at 78% (95% CI 71.8-84.9) vs. 87.8% (95%CI 84.5-91.4) (P<0.01). In multivariate analysis, elevated sPD-L1 (HR=1.75; 95%CI 1.16-2.64), age (HR=1.03; 95%CI 1.02-1.05), high-risk IPI score (HR=3.71; 95%CI 1.91-7.21) and ALC ² 1 G/L (HR=2.19; 95%CI 1.44-3.33) were all significant at P<0.01. In analyses stratified by IPI, the 3-year OS rates among high-risk patients (IPI 4-5) was 40.9% (95% CI 23.6-71.0) for elevated sPD-L1 vs. 82.1% (95% CI 69.1-97.6) for not elevated sPD-L1 (P<0.01). There was no association of sPD-L1 with 3-year OS among low risk (IPI 0-1) or intermediate-risk (IPI 2-3) patients.
Conclusion. We confirmed that sPD-L1 levels are higher in pre-treatment plasma samples of newly diagnosed DLBCL patients compared to controls, and that elevated levels of sPD-L1 are associated with inferior OS in DLBCL patients treated with immunochemotherapy, and this is independent of IPI and other clinical factors. Among high risk patients, we identified a subgroup with less than 50% survival.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal