Abstract
Introduction: Pediatric patients with acute myeloid leukemia (AML) require central nervous system (CNS) directed chemotherapy to minimize CNS relapse. Patients with AML who have CNS disease at diagnosis, defined as >5 white blood cells (WBC) with positive blast in cytospin, require more intensive CNS directed therapy to clear CNS disease and prevent CNS relapse. Those with <5 WBC but with a positive cytospin are designated as CNS2 disease. Those without any blast (negative cytospin) are designated as CNS1. The need for extra CNS therapy for CNS2 patients varies among treatment protocols, and consensus has not been reached as to the best CNS directed therapy for these patients. We studied the impact of intensive vs. standard management of CNS2 patients by comparing patients treated on the two most recent Children’s Oncology Group (COG) trials to those treated on the St Jude Children’s Research Hospital AML02 trial, where COG trials managed those with CNS2 disease more intensively, similar to CNS3, and AML02 treated such patients similar to CNS1. Both trials used a similar MRC-based chemotherapy backbone. This backbone gave intrathecal (IT) cytarabine at the beginning of each cycle of therapy except Capizzi II therapy, and on the AML02 protocol most patients received IT triple therapy. On both backbones, patients with CNS3 disease, and those on COG trials with CNS2 disease, received twice weekly IT cytarabine until the CSF was clear of blasts plus 2 additional treatments with a minimum of 4 IT treatments given. Thus, this analysis is the first comparison of outcome of CNS2 patients examining the variable of additional CNS directed therapy.
Methods: Disease characteristics and clinical outcome for children who were CNS2 treated with intensive or standard intrathecal chemotherapy were compared across COG and SJCRH studies and compared to those who were CNS1 or CNS3.
Results: Among the 1361 eligible patients enrolled on AAML03P1 and AAML0531 with available data for CNS status, 247 had CNS2 status. Of the 200 eligible patients enrolled on AML02, 47 patients had CNS2 status. On all protocols, patients with CNS2 status had a significantly higher incidence of Inv(16) compared to CNS1 patients (p<0.001 for both protocols). As well, patients with CNS2 status had a higher incidence of M4 FAB classification compared to CNS1 patients (p<0.001 for COG protocols and p=0.002 for AML02). On both protocols, patients who were CNS2 had similar incidence of Inv(16) compared to patients who were CNS3. In contrast, on the COG protocols the incidence of M4 FAB was similar among CNS2 and CNS3 patients, while on the AML02 protocol the incidence of M4 FAB was significantly higher in CNS2 compared to CNS3.
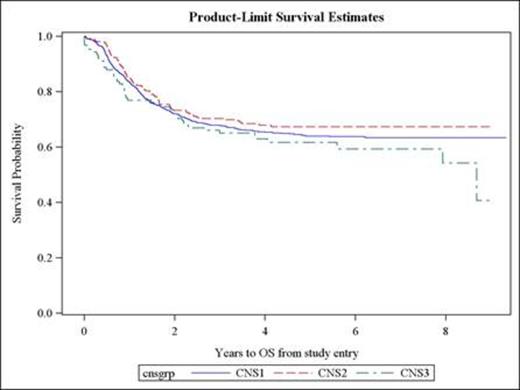
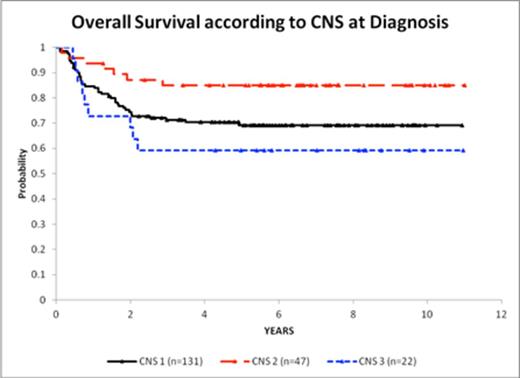
The event free survival (EFS) for patients treated on COG protocols showed significant differences according to CNS status, with CNS1 patients having superior EFS compared to CNS2 and CNS3 patients (p=0.005), while on AML02, the EFS for CNS2 patients was significantly higher than CNS3 patients (p=0.04) and higher, but not significantly, than CNS1 patients (p=0.06). The overall survival (OS) for CNS2 patients treated on COG protocols was not significantly different from that of CNS1 and CNS3 patients (p=0.32), while on AML02, the OS was significantly higher for CNS2 patients compared to CNS1 (p=0.05) and CNS3 patients (p=0.02)(Figures 1 and 2). However, for the AML02 protocol, the Cox analysis showed that CNS status was not independently associated with EFS, OS, or cumulative incidence of relapse
On the COG protocols there were 101 patients with relapse involving CNS, of which 34 were CNS1, 32 CNS2 and 34 CNS3 with a 5 year CNS refractory/relapse rate of 4%, 13% and 28% respectively (p<0.001). One patient with CNS relapse was unknown for CNS group. Of the 101 patients who relapsed involving CNS: 34% were CNS1, 32% were CNS2, and 34% were CNS3.
Conclusions: Patients with AML who have <5 white cells with blasts present in the cerebrospinal fluid at diagnosis may not require extra IT therapy but may be able to be treated in the same fashion as patients with no blasts in the CSF at diagnosis. Additional analyses will assist in determining which, if any, CNS2 patients require extra IT therapy.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal