Abstract
Background: Hemophagocytic lymphohistiocytosis (HLH) is a severe clinical syndrome characterized by the activation of mononuclear phagocytic system. Patients (pts) typically present with fever, cytopenias, splenomegaly, hyperferritinemia and hemophagocytosis. There are two categories of HLH: primary (familial) and secondary (acquired). Primary HLH (FHL) is caused by genetic defects in proteins involved in cytotoxic function in T and NK cells, and occurs most commonly in children; though hypomorphic mutations in the same genes may cause adult-onset FHL. In contrast, secondary HLH typically occurs in adults, and is due to underlying infectious, autoimmune, and malignant disorders. The limited knowledge about secondary adult HLH is derived from case reports or case series involving few pts. The current study is the first collaborative effort to describe the etiology, clinical characteristics and outcomes in a large cohort of adult HLH pts.
Methods: All adult (≥18 years) pts with a diagnosis of HLH according to the HLH-04 criteria seen at Barnes Jewish Hospital, St. Louis, MO (from October 2003 through June 2014) and at Mayo Clinic, Rochester, MN (from January 1996 through May 2014) were identified. Five of the following eight criteria are considered diagnostic of HLH according to the HLH-04 criteria: 1) fever ≥38.50C; 2) splenomegaly; 3) cytopenia of two or three lines: ANC <1 × 109/L, hemoglobin <9 g/dL, platelet count <100 × 109/L; 4) serum triglycerides ≥265 mg/dL or serum fibrinogen ≤150 mg/dL; 5) serum ferritin ≥500 mcg/L; 6) soluble IL-2 receptor ≥2400 U/mL; 7) low/absent NK cell activity; and 8) biopsy-proven hemophagocytosis. Pts who were treated as HLH but did not fulfill the diagnostic criteria were excluded. The most likely etiology of HLH (malignancy, infection, autoimmune, and idiopathic) was assigned for each patient based on standard diagnostic criteria. Clinical characteristics were compared using Chi-square, student’s t-test and Mann-Whitney test, as appropriate. Overall survival (OS), defined as time from HLH diagnosis to death from any cause, was assessed using Kaplan-Meier survival analysis and log-rank tests. The Institutional Review Boards of both institutions approved this study.
Results: One hundred and sixteen adult pts with HLH were identified. Their median age at diagnosis was 50 years (range, 18-82); 69 (58%) pts were male. The clinical and laboratory findings of pts according to HLH-04 criteria are summarized in Table 1. At diagnosis, the median serum ferritin was 18510 mcg/L (range, 561-684,000), median serum fibrinogen was 169 mg/dL (range, 50-766), and median serum triglycerides was 307 mg/dL (range, 68-1475). Ninety-one (78%) pts had transaminitis; 97/106 (92%) pts had hypoalbuminemia; 86/114 (75%) pts had elevated PT and/or aPTT; and 51 (44%) pts had renal insufficiency. The causes of HLH were as follows: 43 (37%) malignancies, 42 (36%) infections, 15 (13%) attributed to autoimmune disorders and primary immunodeficiencies, and 16 (14%) were idiopathic.
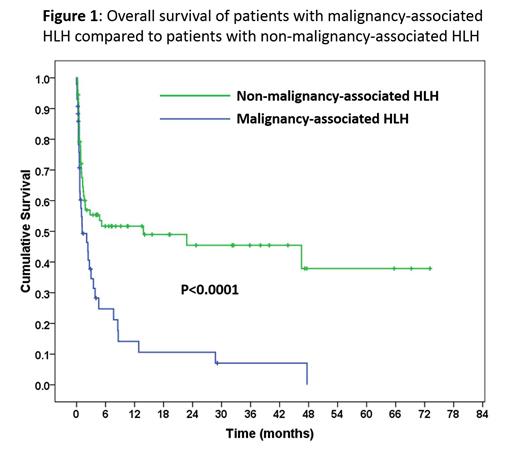
After a median follow-up of 1.5 months, 70 (60.3%) pts have died. The median OS of the entire cohort was 2.8 months (range, 0.1-73.1 months), with a 5-year overall survival of 20%. Pts with malignancy-associated HLH had a markedly worse survival (median=1.2 months) compared to pts with non-malignancy-associated HLH (median=13.8 months, p < 0.0001, Figure 1). In a multivariable analysis, malignancy-associated HLH (hazard ratio [HR] = 4.4; 95% CI: 1.7-11.3; p = 0.002) and male gender (HR = 2.8, 95% CI: 1.2-6.5; p = 0.02) were independently associated with shorter survival.
Conclusions: The triad of fever, cytopenias and elevated ferritin (present in >80% of pts in this series) should alert physicians to a possible diagnosis of adult HLH. Survival after a diagnosis of HLH is dismal, especially among those with malignancy-associated HLH. The development of a national registry for adults with HLH will be beneficial to further our understanding of this condition and develop effective treatment strategies.
Clinical and laboratory findings according to the HLH-04 criteria
| Characteristic . | No. (%) of patients . |
|---|---|
| Fever | 112/116 (97) |
| Splenomegaly | 75/116 (65) |
| Bicytopenia or pancytopenia | 95/116 (82) |
| Hypertriglyceridemia | 71/107 (66) |
| Hypofibrinogenemia | 50/107 (47) |
| Hemophagocytosis | 95/111 (86) |
| Hyperferritinemia | 115/115 (100) |
| Elevated soluble IL-2 | 33/40 (82) |
| Absent or decreased NK cell function | 12/22 (54) |
| Characteristic . | No. (%) of patients . |
|---|---|
| Fever | 112/116 (97) |
| Splenomegaly | 75/116 (65) |
| Bicytopenia or pancytopenia | 95/116 (82) |
| Hypertriglyceridemia | 71/107 (66) |
| Hypofibrinogenemia | 50/107 (47) |
| Hemophagocytosis | 95/111 (86) |
| Hyperferritinemia | 115/115 (100) |
| Elevated soluble IL-2 | 33/40 (82) |
| Absent or decreased NK cell function | 12/22 (54) |
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal