Abstract
Background and Aim: The emergence and dissemination of Carbapenemase producing Klebsiella pneumoniae (KPC) represent a serious threat to public health and is associated with high mortality rates in patients with hematologic malignancies. Several risk factors (prior exposure to or current use of antibiotics, extended stay in hospital, neutropenia, sharing a room with a know carrier etc) have been identified for colonization in hematological patients. However, data on how to contain their spread in haematological setting are still surprisingly limited. We carried out a prospective investigation to assess the prevalence of KPC colonization among hematologic patients, the impact of a strategy control to limit the spread and to evaluate the efficacy of an implementation of more extensive active surveillance.
Methods: Infections caused by multiresistant pathogens have been recorded in our Unit from January 2012 through June 2014. From January 2012 to July 2013, we developed an intensive control infection program, (Plan A): 1. Weekly colonization screening for KPC; 2. Educate healthcare personnel about KPC; 3. Promotion of hand hygiene 4. Physical separation of carriers from non-carriers 5. A double-carbapenem plus colistin therapeutic empiric regimen was given for blood stream infections. Since July 2013, we decided to implement additional measures, including (Plan B): 1. Drastic reduction in the number of beds. 2. 2% chlorhexidine body washing for colonized patients. 3. Ensure access to adequate hand hygiene stations (i.e., clean sinks and/or alcohol) and ensure they are well stocked with supplies (e.g. towels, soap, etc.) 4. Donning gown and gloves before entering the affected patient’s room and removing the gown and gloves and performing hand hygiene prior to exiting the affected patient’s room.
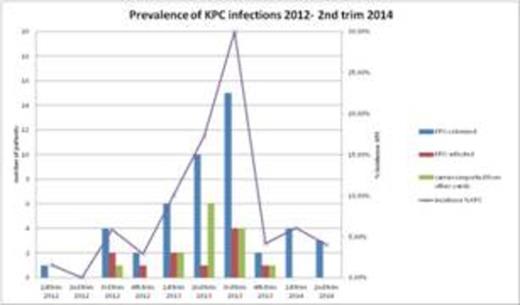
Results: Since January 2012 perianal swabs were detected weekly from 607 consecutive patients affected by hematologic malignancies, for a total of 1079 admissions and 12.284 days of hospital stay.KPC colonization was present in 47 out of 607 (7.7%) screened patients at some time during their (often multiple hospitalizations); 11 bloodstream infections were reported in 9 patients (23%). Three deaths (3/11, 27%) due to KPC were reported before implementation screening (overall mortality rate was 6.3 % of colonized patients). KPC-decolonisation was achieved in 13/47 pts (28 %) after a median duration of 88 days (range 20-118).Most patients who recovered from KPC infection or were just colonized by KPC went on to receive additional chemotherapy without any life threatening KPC infection occurring (only one patient reported two septic episodes). Since screening cultures or further clinical cultures identified a progressive increase KPCcolonized or -infected patients, we decided to implement additional measures (Plan B). Therefore, from fourth trimester 2013 of study, we have observed a progressive decrease in rate of new colonization: 2 patients (4.17%) vs 15 patients (30%) in the third trimester, and a very low rate was maintained until the second trimester of 2014( 3 patients -4%).
Conclusions: The prevalence of KPC colonization in our hospital is high among patients with hematologic diseases.An implementation of additional measures, sharing the patients in single bed-rooms and consequently limiting transfer of cases from other wards, was able to contain KPC colonization and infection.However, the success of our preliminary interventions should be monitored constantly; besides, to prevent the emergence and further spread of CRE, a coordinated regional control effort among healthcare facilities should be recommended.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal