Abstract
Background: There is a significant variation in disease incidence and outcomes among Multiple Myeloma (MM) patients (pts) from different ethnic backgrounds. Currently, there is a paucity of data regarding the influence of demographics and ethnicity on behavioral patterns of pts, their attitudes, beliefs, and knowledge about MM and its treatment, which could in turn affect outcomes. We conducted a questionnaire-based study to examine behavioral patterns of MM pts, especially focusing on ethnic minorities and how this may impact patient awareness and symptom complex related to the disease and its treatment.
Methods: Apaper-basedquestionnaire consisting of 61 questions encompassing four broad categories was provided to participating pts at the University of Southern California Medical Centers. These included demographics, disease/treatment related quality of life (QoL), satisfaction regarding treatment, and satisfaction regarding treating physician/healthcare staff. Information on clinical characteristics and MM-related treatment was collected through an IRB-approved protocol. Pts were stratified by age, gender, and ethnicity (Hispanics vs. Non-Hispanics). Any missing patient responses were withdrawn from the final analysis of that question. Categorical and continuous variables were compared among groups using Chi-square and Kruskal-Wallis tests, respectively. All statistical analysis utilized SAS software (v9.3) with a two-sided significance level of 0.05.
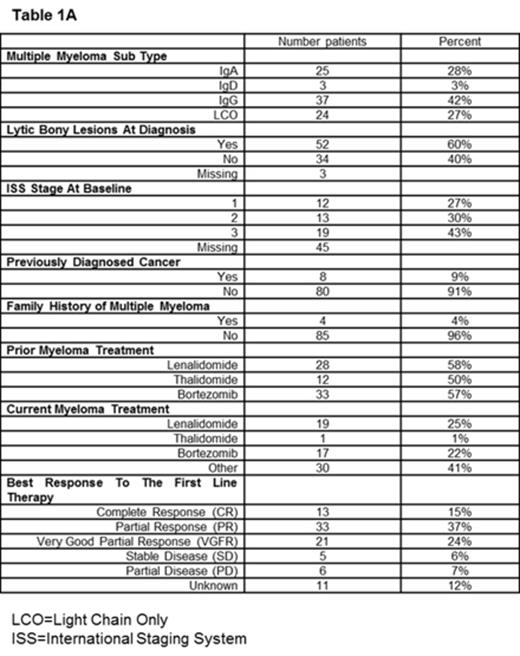
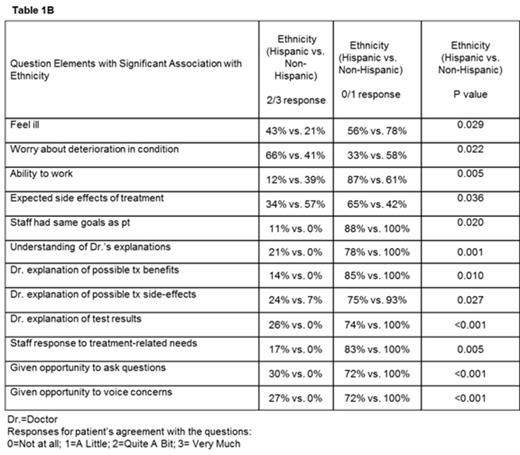
Results: A total of 89 pts (males: 40, females: 49) from March 2012 to October 2013 responded to the questionnaire of the 100 pts that were consented (81%). Median age was 59 (range: 23-81) years and 43 (48%) pts were Hispanic while 46 (52%) were Non-Hispanic. Baseline clinical characteristics are shown in Table 1A. As compared to Non-Hispanics, Hispanic pts were less likely to have completed college (70% vs. 30%, p<0.001), attend myeloma support groups (90% vs. 10%, p=0.026), feel they had sufficient disease/treatment-related information (72% vs. 22.5%, p<0.001). Hispanic pts were more likely to report being unemployed/without any income (57.5% vs. 9%, p<0.001), have 3-4 people living in the house (57.5% vs. 26 %, p=0.009), feeling ill (43% vs. 21%, p=0.029), have concern about deterioration in clinical condition (66% vs. 41%, p=0.022), and inability to work due to symptoms from MM or its treatment (38.6% vs. 11.9%, p=0.005) when compared to Non-Hispanics. With respect to MM treatment, Hispanic pts were less likely to report that side effects were as expected (34% vs. 57%, p=0.036) and believe that treating staff worked towards the same goal (88% vs. 100%, p=0.020) as them. Hispanic pts also reported a lower level of satisfaction with their doctor /treatment staff, as compared to Non-Hispanic pts and this difference was statistically significant as shown in Table 1B. Using gender as the stratification factor, we noted that female pts were more likely to report lack of energy (p=0.037), pain (p=0.010), satisfaction with discussion on emotional health (p=0.012) as compared to males. With age as the stratification factor, patients < 60 years of age were less likely to report expected effectiveness from treatment (p=0.031), satisfaction regarding appropriateness of treatment (p=0.008) or explanation of test results by their doctor (p=0.036), and were more likely to worry about deterioration in their condition (p=0.014). We did not find a statistically significant association between age, gender, or ethnicity and response to initial myeloma treatment.
Conclusions: We found a significant association between MM patient ethnicity and the pts responses to questions pertaining to their QoL, satisfaction with treatment and treating physician. This difference in disease/treatment related knowledge and attitudes may be related to socio-cultural and behavioral patterns and may contribute to factors such as treatment compliance, effectiveness and symptom complex burden amongst others, that can impact outcomes among ethnic subgroups of MM pts. Efforts to mitigate these differences should focus on improving methods of patient education, spread more awareness among ethnic minorities, integration of psychosocial care into cancer therapy and promoting health psychology research.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal