Abstract
Introduction
The outcome and the role of allogeneic hematopoietic cell transplantation (Allo-HCT) with reduced-intensity conditioning (RIC) in patients with nodal peripheral T-cell lymphomas (PTCLs) remain unclear.
Patients and Methods
To address this issue, we retrospectively analyzed the outcome of Allo-HCT for patients with nodal PTCLs using the transplant registry data from the Japan Society for Hematopoietic Cell Transplantation (JSHCT).
Patients who fulfilled the following criteria were included in this study: aged 16-69 years, diagnosed with PTCL not otherwise specified (PTCL-NOS), angioimmunoblastic T-cell lymphoma (AITL), or anaplastic large cell lymphoma (ALCL), and received the first Allo-HCT in Japan between January 1, 2001 and December 31, 2011.
In this analysis, conditioning regimen intensity was the main variable of interest. The conditioning regimen was classified as myeloablative conditioning (MAC) if it included total body irradiation (TBI) > 8 Gy, oral busulfan (BU) ≥ 9 mg/kg, intravenous BU ≥ 7.2 mg/kg, or melphalan (MEL) > 140 mg/m2. Otherwise, it was classified as RIC.
Results
A total of 354 patients (200 PTCL-NOS, 77 AITL, and 77 ALCL) were analyzed. Median follow-up duration of surviving patients was 3.8 years. Donor sources consisted of 122 human-leukocyte-antigen (HLA)-matched bone marrow (BM)/peripheral blood (PB), 122 HLA-mismatched BM/PB, and 110 cord blood.
Of the 354 patients, 146 (41.2%) received MAC, which consisted of cyclophosphamide (CY)-TBI-based (n = 84), other TBI-based (n = 24), BU-CY-based (n = 11), fludarabine (FLU)-BU-based (n = 10), FLU-MEL-based (n = 15), and other (n = 2) MAC. The remaining 208 (58.8%) patients received RIC, which consisted of FLU-BU-based (n = 62), FLU-MEL-based (n = 108), and other (n = 38) RIC.
Comparison of the patients who received MAC and RIC revealed that the RIC patients were significantly older (median age: 40.5 years vs. 50.3 years; P < 0.001) and more likely to have received autologous-HCT prior to Allo-HCT (15.1% vs. 29.3%; P = 0.002).
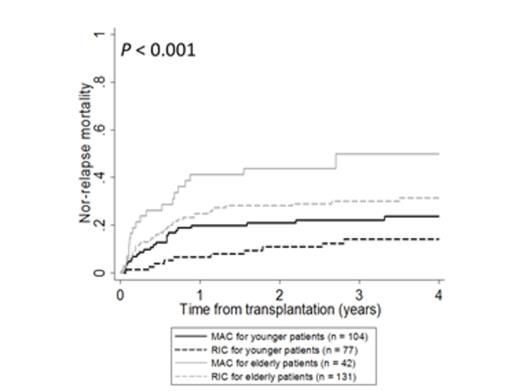
The unadjusted 3-year cumulative incidence of non-relapse mortality were following: younger patients receiving MAC, 22%; younger patients receiving RIC, 14%; elderly patients receiving MAC, 50%; elderly patients receiving RIC, 30% (P < 0.001; Figure 1). The multivariate analysis showed that patients receiving RIC had a significantly lower non-relapse mortality than patents receiving MAC (HR, 0.51; 95% CI, 0.32-0.80; P = 0.004).
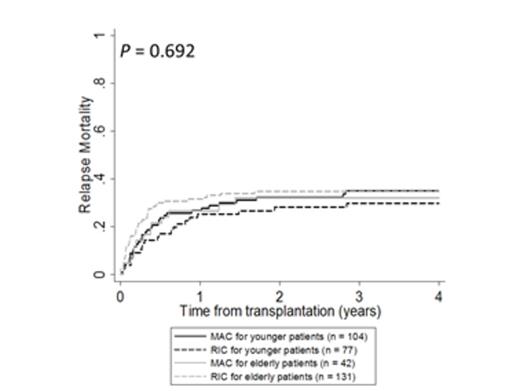
The unadjusted 3-year cumulative incidence of relapse mortality were following: younger patients receiving MAC, 35%; younger patients receiving RIC, 30%; elderly patients receiving MAC, 32%; elderly patients receiving RIC, 35% (P = 0.692; Figure 2). The multivariate analysis showed that patients receiving MAC and RIC had a comparable relapse mortality (HR, 1.08; 95% CI, 0.73-1.58; P = 0.711).
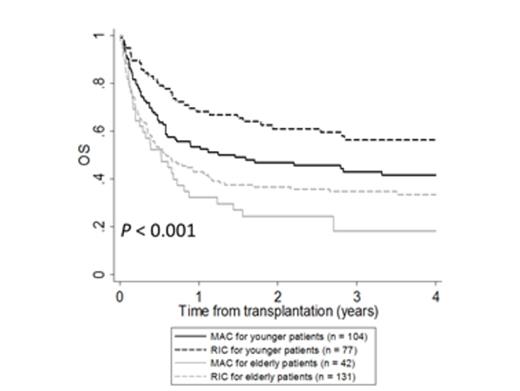
The unadjusted 3-year overall survival rates were following: MAC for younger patients (aged 16-49 years), 43%; RIC for younger patients, 56%; MAC for elderly patients (aged 50-69 years), 18%; RIC for elderly patients, 35% (P < 0.001; Figure 3). The multivariate analysis showed that patients receiving RIC had a significantly superior overall survival than patients receiving MAC (HR, 0.74; 95% CI, 0.54-1.00; P = 0.047; Table I).
Multivariate analysis for overall survival
| . | Overall Survival . | . |
|---|---|---|
| HR (95% CI) | P value | |
| Conditioning Regimen | ||
| myeloablative | 1.00 | - |
| reduced-intensity | 0.74 (0.54-1.00) | 0.047 |
| Patient Age | ||
| 16 to 34 | 1.00 | - |
| 35 to 49 | 1.26 (0.83-1.91) | 0.270 |
| 50 to 59 | 2.17 (1.46-3.23) | < 0.001 |
| 60 to 69 | 2.24 (1.40-3.59) | 0.001 |
| Karnofsly Performance Status | ||
| 90 to 100 | 1.00 | - |
| 10 to 80 | 2.02 (1.41-2.91) | <0.001 |
| missing | 1.50 (1.07-2.10) | 0.017 |
| Disease Status | ||
| complete remission | 1.00 | - |
| partial remission | 1.13 (0.71-1.82) | 0.607 |
| resistant relapse | 2.02 (1.27-3.21) | 0.003 |
| primary induction failure | 2.09 (1.33-3.27) | 0.001 |
| . | Overall Survival . | . |
|---|---|---|
| HR (95% CI) | P value | |
| Conditioning Regimen | ||
| myeloablative | 1.00 | - |
| reduced-intensity | 0.74 (0.54-1.00) | 0.047 |
| Patient Age | ||
| 16 to 34 | 1.00 | - |
| 35 to 49 | 1.26 (0.83-1.91) | 0.270 |
| 50 to 59 | 2.17 (1.46-3.23) | < 0.001 |
| 60 to 69 | 2.24 (1.40-3.59) | 0.001 |
| Karnofsly Performance Status | ||
| 90 to 100 | 1.00 | - |
| 10 to 80 | 2.02 (1.41-2.91) | <0.001 |
| missing | 1.50 (1.07-2.10) | 0.017 |
| Disease Status | ||
| complete remission | 1.00 | - |
| partial remission | 1.13 (0.71-1.82) | 0.607 |
| resistant relapse | 2.02 (1.27-3.21) | 0.003 |
| primary induction failure | 2.09 (1.33-3.27) | 0.001 |
Conclusion
We showed a favorable outcome of Allo-HCT with RIC in patients with nodal PTCLs. The efficacy of RIC Allo-HCT for nodal PTCLs needs to be explored in prospective study.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal