Abstract
Autologous or allogeneic hematopoietic stem cell transplantation (SCT) is considered in an attempt to improve survival in patients with relapsed or refractory lymphoma. The major problem with allogeneic transplantation is the increased treatment-related mortality (TRM) in comparison to autologous transplantation but some evidence supports the existence of a graft-versus-lymphoma (GVL) effect in lymphoblastic lymphoma with allogeneic SCT. Pediatric mature B-cell Non-Hodgkin lymphoma (B-NHL) is highly curable with intensive chemotherapy. It is hard to evaluate the role of autologous or allogeneic SCT in the era of modern chemotherapy regimens and the evidence for a potent GVL effect in B-NHL is not convincing. Therefore, we undertook a retrospective study of patients who underwent either autologous or allogeneic transplantation and analyzed the effect of several important factors, including donor source and survival rate, using the national registry data (Transplant Registry Unified Management Program; TRUMP).
This study includes patients with B-NHL aged 18 years and younger who underwent single SCT facilitated by the TRUMP from 1990 to 2012. TRUMP system was established to unify of hematopoietic SCT registries in Japan. Primary end points were overall survival (OS), relapse, and TRM. TRM was defined as death during a continuous complete remission or death in the first 28 days after transplantation.
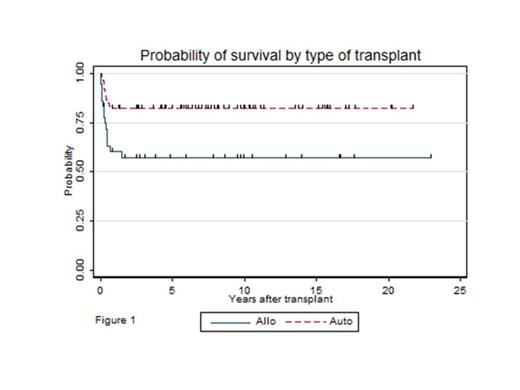
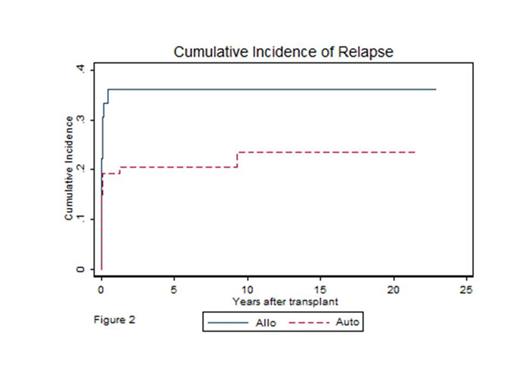
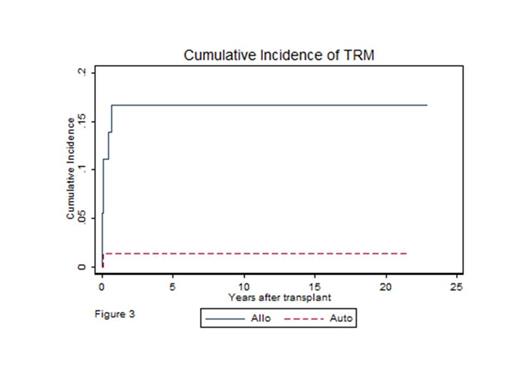
There were 73 autologous transplantations and 36 allogeneic bone marrow transplantations available for analysis. Among the patients with autologous SCT, 8 underwent bone marrow transplantations and 65 underwent peripheral blood stem cell transplantations. Autologous transplant recipients were more likely to receive early transplants after diagnosis, more likely to receive transplants before 1999, less likely to be stage IV, and less likely to receive a TBI-containing conditioning regimen than allogeneic transplant recipients. With a median follow-up time of 5.9 years, the probabilities of OS were 57% (95% CI, 49%-66%) after allogeneic transplantation and 82% (95% CI, 78%-87%) after autologous transplantation (p = 0.004; Figure 1). Multivariate analysis confirmed that OS was significantly worse with allogeneic SCT (HR = 3.12, 95% CI, 1.01-9.69, p = 0.049), adjusted by the time from diagnosis to SCT, disease status at transplant, year of transplant, stage of lymphoma, and use of TBI. Cumulative incidence of relapse by type of transplant, showed no statistically significant difference after autologous versus allogeneic transplantation (p = 0.099; Figure 2). Seven patients died of transplant related complications including patients in the allogeneic SCT (n = 6) and autologous SCT (n = 1) groups. The causes of death were infection (n = 3), disease progression in the first 28 days after SCT (n = 3) and chronic graft-versus-host disease (n = 1). The 6-year cumulative incidences of TRM were 17% (95% CI, 6.8%-30%) after allogeneic transplantation and 1.4% (95% CI, 0.1%-6.6%) after autologous transplantation (p < 0.001, Figure3). There were too few events in the transplants to permit multivariate analysis. At every time point following transplantation, allogeneic transplant recipients were significantly more likely to die of treatment-related causes than autologous transplant recipients.
In pediatric B-NHL, OS was significantly worse for allogeneic than for autologous SCT due to higher TRM with allogeneic SCT recipients. We have not found differences in the relapse rate between allogeneic and autologous SCT. Because TRM was the most important cause of treatment failure for the allogeneic patients, strategies to reduce TRM without compromising the GVL effect may be useful in pediatric B-NHL with SCT.
Fujita:Japan Leukemia Research Fund: Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal