Abstract
Introduction: Allogeneic hematopoietic cell transplantation (HCT) has curative potential for a variety of hematologic malignancies. However, the success of HCT is heavily dependent on the disease and remission status. Armand et al. recently proposed a disease risk index (DRI) to assess the risk for allogeneic HCT based on the disease and remission status, and could be used to risk stratification on survival (Armand et al Blood 2012), but evaluation of its clinical significance is limited. HCT-comorbidity index (HCT-CI) was developed as a measure of pretransplant organ dysfunctions (Sorror et al Blood 2005), which has been shown to be associated with nonrelapse mortality (NRM). In order to clarify any association between pretransplant factors including DRI and HCT-CI, and respective overall survival (OS), NRM and relapse rate, we retrospectively reviewed the data of patients who underwent allogeneic HCT at our department.
Patients and Methods: A total of 305 patients with hematologic malignancies who underwent initial allogeneic HCT at our department between January 2000 and April 2013 were included. After excluding patients with insufficient HCT data, we included a total of 244 patients (138 male, 106 female) with a median age of 49.5 (range 15-69) years. A total of 133 patients received myeloablative conditioning and 111 received reduced-intensity regimens. Stem cell sources were bone marrow (n=177), peripheral blood (n=32), combined peripheral blood and bone marrow (n=1), and cord blood (n=34). A total of 146 patients received tacrolimus-based regimens and 98 patients received cyclosporine-based regimens for GVHD prophylaxis. The DRI has four risk-based categories (low, intermediate, high, and very high) and the HCT-CI has three categories in order of ascending risk (0, 1-2 and ≥3). OS was calculated with the Kaplan-Meier method, compared among groups with the log-rank test, and multivariable Cox regression analyses were used to evaluate factors associated with OS. The cumulative incidence of NRM and relapse were calculated while treating relapse and death without relapse, respectively, as competing events, and competing risk regression analyses were used to evaluate risk factors associated with NRM and relapse.
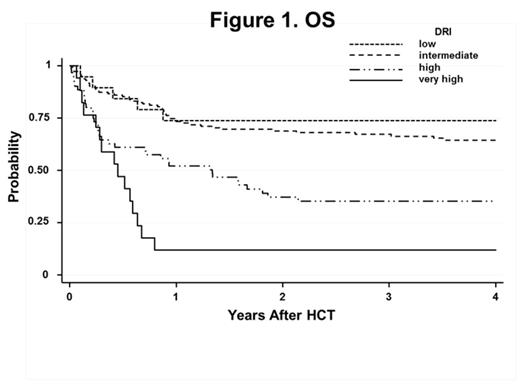
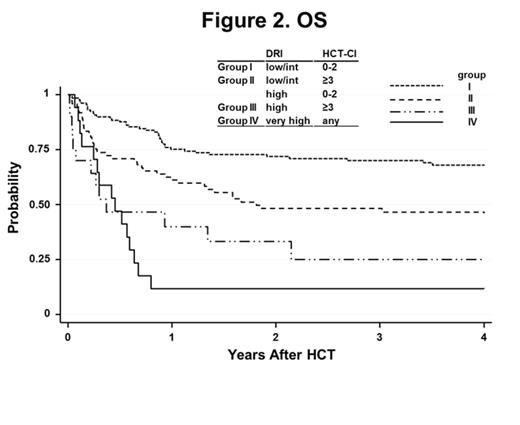
Results: The median follow-up for survivors was 4.7 years (range 0.1-14.2 years). Pretransplant disease risks in the DRI low, intermediate, high, and very high risk groups were 8%, 60%, 25%, and 7%, and 4-year OS in the same groups were 74%, 64%, 35%, and 12%, respectively (Figure 1, p<0.001). Four-year OS among patients with a HCT-CI of 0, 1-2, and ≥3 were 63%, 52%, and 41%, respectively. Multivariable analysis showed a significant association with OS for DRI (high risk hazard ratio [HR] 2.62, p<0.001; very high risk HR 5.26, p<0.001 versus intermediate risk), HCT-CI (HCT-CI ≥3 HR 1.64, p=0.022 versus HCT-CI 0-2), 2-4 performance status (HR 3.10, p<0.001), and donor-recipient ABO minor-mismatch (HR 2.00, p=0.005 versus ABO match). The cumulative incidence of 4-year NRM was 25%, and NRM was significantly associated with HCT-CI (HCT-CI ≥3 HR 2.27, p=0.003 versus HCT-CI 0-2) and 2-4 performance status (HR 3.89, p<0.001). The cumulative incidence of 4-year relapse was 25%, and relapse was significantly associated with DRI (high risk HR 2.26, p=0.012; very high risk HR 8.11, p<0.001 versus intermediate risk). Finally, we reclassified all patients into four risk groups incorporating DRI and HCT-CI: DRI low-intermediate plus HCT-CI 0-2 (group I), DRI low-intermediate plus HCT-CI ≥3, or DRI high plus HCT-CI 0-2 (group II), DRI high plus HCT-CI ≥3 (group III), and DRI very high (group IV). Four-year OS among patients with group I, II, III, and IV were 68%, 47%, 25%, and 12%, respectively (Figure 2, p<0.001).
Conclusions: Our results suggest that risk stratification with DRI and HCT-CI for the prognosis of relapse and NRM may be useful for patients undergoing allogeneic HCT. Larger and prospective studies are warranted to more precisely validate these findings.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal