Abstract
Treatment-response assessment via quantification of MRD has become a corner-stone for risk stratification in childhood ALL. Although MRD has been shown to retain independent prognostic significance, the relationship with other prognostic variables has been incompletely explored. Moreover, determination of the most reliable treatment time-point for FCM-MRD evaluation that would serve as the best surrogate marker in predicting relapse, is still an issue of debate. To determine the utility of sequential measurements of FCM-MRD, with specific emphasis on day 33 and its correlation with known prognostic factors and outcome, we retrospectively analyzed the results of FCM-MRD study/data of 825 bone marrow samples of 133 children with ALL, at different treatment time-points, during induction and early consolidation (days 15, 33, 78, week 22-24, at start and at the end of maintenance therapy). All patients were homogeneously treated on BFM-based protocols and prognostic groups were defined by sex, WBC, prednisone response, risk-group allocation, immunophenotype and ETV6/RUNX1-presence. We investigated: a) the relationship between relapse probability and known prognostic factors like age, sex, WBC, immunophenotype, prednisone-response, ETV6/RUNX1 translocation, CDKN2A/2B deletion, hyperdiploidy, protocol risk-group, MRD(constant variable) and MRD positivity(≥0.1% vs <0.1%)(Kaplan-Meier and lïgrank test), b) the correlation between MRD(+) and outcome (OS and EFS, Kaplan-Meier). Additionally, multivariable Cox-models were used to determine the impact of MRD and WBC, sex, age, prednisone-response, on OS and EFS.
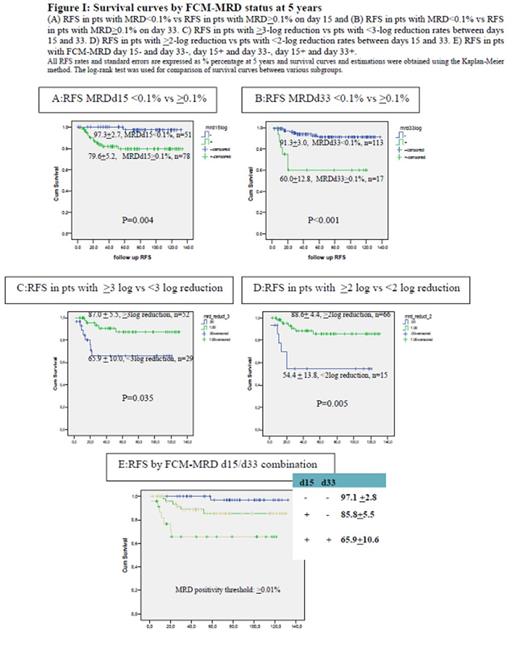
Patients with MRD≥0.1% at the end of induction (day 33) were estimated with 5-year RFS rates of only 60.0±12.8%, compared to MRD low(<0.1%)/negative patients that enjoyed superior 5-year RFS rates of 91.3±3.0%. Both days 15 and 33 of FCM-MRD positivity maintained a significant prognostic impact on the incidence of relapse within all subgroups. MRD(+)d15 and MRD(+)d33 detection combined, appeared to have a statistically significant impact on survival probability (RFS 65.9%±10.6, p<0.001). Additionally, FCM-MRD on day 33 was notably more strongly associated with used prognostic factors, while we were able to demonstrate that FCM-MRD log-reduction rates between days 15 and 33 can also be added as an important relapse prediction marker, apart from absolute MRD quantifications.
In our study, MRD(+)d15 and MRD(+)d33 in combination, strongly and statistically significant correlated with survival probability. Additionally, we propose the FCM-MRD log-reduction rate between days 15 and 33 and end-induction evaluation(day 33) as better predictors of survival and relapse probability, than only day 15 FCM-MRD estimations.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal