Abstract
Background: Despite improvements in supportive care, treatment of AML remains associated with complications. We have developed a multivariate model – the Treatment-Related Mortality (TRM) score – which includes age, performance status, and 6 other covariates to predict 28-day mortality with c-statistic = 0.82 (1.0 = perfect prediction, 0.5 = no prediction) (Walter et al. J Clin Oncol 2011). We investigated associations between TRM score and complications developing during AML treatment.
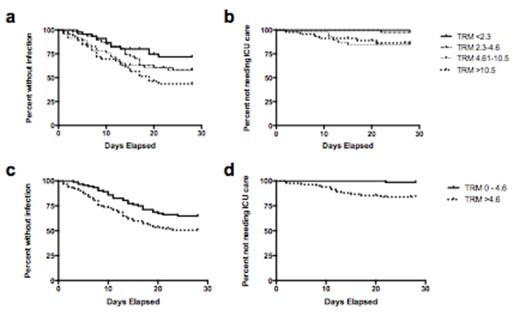
Patients and Methods: 179 adults (median age 53 [range: 18-77] years) with newly diagnosed AML treated at our institution from 2002-2012 with 7 + 3 or similar therapy were included. Documented infections, ICU transfer, and death until the earlier of day 28 or administration of additional chemotherapy were recorded. Patients were categorized by quartiles of TRM score. All outcomes were treated as time-to-event endpoints. The survival probabilities in the absence of infection or ICU transfer were estimated using the Kaplan-Meier method; the 10 patients in the ICU at the start of chemotherapy were excluded from analysis of ICU transfer as an adverse event. Outcomes between TRM scores by quartile were assessed using log-rank test for trend; scores above and below the median were compared using Cox regression. Multivariate models were adjusted for gender, cytogenetic risk, baseline absolute neutrophil count, and year of treatment.
Results: The median TRM score was 4.6 (quartiles 2.3 and 10.5). Documented infections occurred in 72 patients (40%), ICU transfer in 14 (8%), and death in 4 (2%) within 28 days of induction. Patients with higher ranges of TRM scores were more likely to develop infections (Ptrend=0.006; Fig 1a) and require ICU transfer (Ptrend=0.003; Fig 1b). In particular, TRM scores above the median were associated with increased risk of infection (P=0.02; Fig 1c) and ICU transfer P=0.0004; Fig 1d). After multivariable adjustment, the risk of documented infection was 1.72 (95% CI: 1.06-2.81)-fold higher for patients with TRM >4.5. Consistent with our recent analysis, baseline grade 4 neutropenia was also independently associated with infection (HR 2.2 [95% CI: 1.38-3.52]) (Buckley et al. Am J Hematol 2014). There was only one ICU transfer, and there were no deaths among the 92 patients with TRM score less than the median. Although supportive care measures have improved in recent years, a high TRM score was still associated with ICU transfer in the subset of patients treated from 2007-2012 (P=0.001).
Conclusions: The TRM score is associated not only with death, but also with other early adverse events. A cut-point of 4.5, which will need to be confirmed in an independent study cohort, may separate low- from high-risk patients in terms of susceptibility to infection and likelihood of requiring an ICU transfer. The TRM score may thus improve assessment of the risks of intensive induction chemotherapy and help allocate health care resources.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal