Abstract
Background: Among Chronic Lymphocytic Leukemia (CLL) patients (pts), 4-10% are diagnosed with autoimmune cytopenias (AC) at some point during the course of their disease. This is less common than cytopenias related to bone marrow infiltration (10-20%). Infiltrative cytopenias (IC) are clearly a poor prognostic factor. However, the effect of AC on survival and prognosis of CLL pts remains understudied.
Objectives: To determine the prevalence of AC and IC among CLL pts and their effect on overall survival (OS) and time to first treatment (TTFT) compared to patients without cytopenia. Furthermore, the effect of different treatment modalities including chemotherapy and chemo-immunotherapy on the disease course was evaluated in patients with AC.
Methods: A population-based retrospective analysis through an electronic search of pts within the Providence Health Care CLL database between 1978 and 2013 was carried out. The diagnostic criteria for autoimmune hemolytic anemia (AIHA) were positive direct antiglobulin test and laboratory evidence of hemolysis, for immune thrombocytopenia (ITP) the exclusion of other etiologies of thrombocytopenia and for pure red cell aplasia (PRCA) anemia with low reticulocyte count and bone marrow evidence of decreased erythropoiesis. Infiltrative cytopenia diagnosis was confirmed by bone marrow biopsy based on lymphocyte percentage and cellularity. Anemia was defined as hemoglobin <100 g/L. Thrombocytopenia was defined as platelets <100 x 109/L. Baseline features of pts with AC and IC were compared using Chi-squared analysis for categorical and the Kruskal-Wallis test for continuous variables. Overall survival was calculated from the date of initial treatment to the date of death from any cause. Time to first treatment (TTFT) was defined as the time interval between the date of diagnosis and date of first CLL treatment. Survival analysis was performed by the Kaplan–Meier method using IBM SPSS statistics for windows.
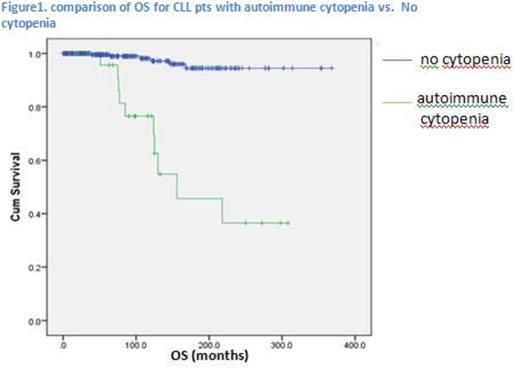
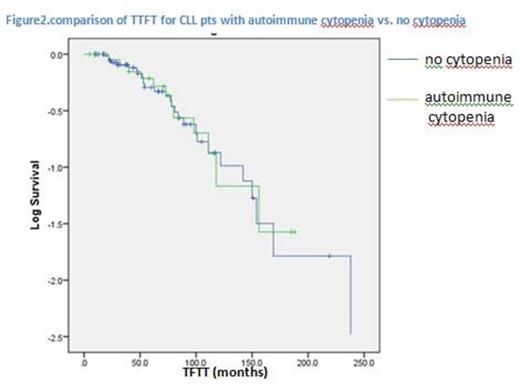
Results: Among 754 pts with CLL, 80 (10.6%) developed cytopenias (anemia and thrombocytopenia). Of those, 50 (6.6%) had IC and 30 (4%) had AC. There was no significant difference between the 2 groups in terms of age, gender, hemoglobin, platelets, LDH, WBC and lymphocyte count at diagnosis. The time to development of cytopenias for the IC and AC groups was similar with median of 3 and 4 years (yrs) from diagnosis, respectively. Within the AC group 16 pts had AIHA, 8 had ITP, 5 had both (Evan's Syndrome) and 1 had PRCA. The median OS was 12.2 yrs (5.9–18.3) and 13 yrs (1.6-24.3) for IC and AC, respectively (p=0.260). However, when compared to CLL pts without cytopenias (median not reached), the AC group had worse OS (p< 0.005) (Fig 1). For the IC and AC groups, the median TTFT was 6.5 yrs (4.5-8.5) and 8.2 yrs (4.1–12.3), respectively (p=0.191). For the CLL pts without cytopenias TTFT was 8.1 yrs (2-12.2), similar to the AC group (p=0.88) (Fig 2). For AC pts, the OS was not significantly different based on treatment received: alkylator based therapy vs. chemo-immunotherapy (p= 0.885). The effect of concomitant hypo-gammaglobulinemia on OS and treatment outcome was studied.Of the 30 pts with AC, 26 had a serum protein electrophoresis done. Of those, 10 (38.5%) had normal results and 16 (61.5%) had low gammaglobulin levels (IgG< 6 g/L); the mean OS was 18.1 yrs and 15.7 yrs respectively (median not reached), (P=0.433).
Conclusion: The prognosis of pts with autoimmune and infiltrative cytopenias was similar.However, CLL pts with AC had worse OS compared to those without cytopenias. There was no significant difference in TTFT between AC and IC or when compared to CLL pts without cytopenias. For the AC group, neither treatment with chemotherapy vs. chemo-immunotherapy nor having concomitant hypo-gammaglobulinemia had an effect on outcome. To our knowledge, there are limited population based studies addressing the importance of determining the etiology of cytopenias in CLL pts and the effect of AC on survival. CLL immune complications need to be studied further especially in the context of novel agents and their effects on immune reconstitution.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal