Abstract
Genes Involved in Maintaining the Bone Marrow Stroma Are Dysregulated in Patients with Myelofibrosis: Lenalidomide Treatment Upregulates SOCS3
Background: Primary myelofibrosis (PMF) is the most aggressive of the myeloproliferative neoplasms (MPNs), a group of genetically and clinically heterogenous yet-related diseases with a functionally disturbed hematopoietic niche. Egress of these cells from the BM in patients with PMF, suggests a change in the crosstalk between hematopoietic stem cells (HSCs) and the BM microenvironment (particularly BM stromal cells). Lenalidomide, an immunomodulatory agent, which modulates inflammatory cytokine secretion, angiogenesis and the expression of adhesion molecules, likely has effects on the BM microenvironment.
Methods: We studied the expression of a set of genes involved in the organization of the hematopoietic niche in peripheral blood and bone marrow (BM) mononuclear cell (MNC) samples from 32 patients with PMF who participated in a phase 2 trial of lenalidomide plus prednisone (Quintas-Cardama et al., J Clin Oncol 2009;27:4760-766). Sequential samples taken at 3, 6, 9, 12 and >14 months after starting lenalidomide therapy were also analyzed. Baseline BM samples were available for 9 patients and baseline PB samples available for 12 patients and used for our analysis. Quantitative reverse transcriptase-polymerase chain reaction was performed to measure the expression levels of SPARC, COX-2, CXCR4, Pax5C-terminus, SOCS3 and HIF-1a transcripts. β-actin was used as an internal control. In addition, we compared the gene expression levels at baseline with healthy control samples.
Results: We found that at baseline (before treatment) COX-2 was upregulated, while CXCR4, Pax5 C-terminus, SOCS3 and HIF-1a were downregulated when compared with expression in healthy BM MNCs. Expression of SPARC, K-RAS,FOS and SOCS2 were not significantly different. In addition, there were no significant differences in relative gene expression between BM MNC and PB samples. We found no correlation between gene expression and JAK2 mutational status or cytogenetic abnormalities. Treatment with LP significantly increased the expression of SOCS3, suggesting that some of the clinical effects of lenalidomide (i.e., reduction in splenomegaly) may be due to a SOCS3-mediated reduction in JAK signaling.
Conclusions: Upregulation of COX-2 and downregulation of CXCR4, Pax5C, SOCS3, and HIF-1a may reflect disruptions in the interactions between cells in the BM microenvironment in MF. Increases in SOCS3 expression upon treatment with lenalidomide may lead to reduced JAK-STAT signaling, which may account for some of its clinical effects in myelofibrosis.
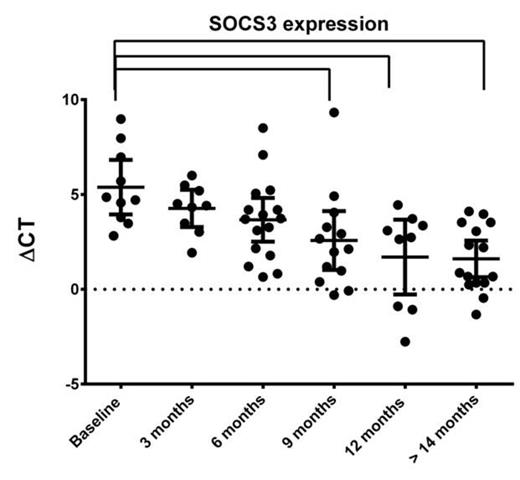
Changes in SOCS3 gene expression with time on lenalidomide plus prednisone treatment. Expression of SOCS3 increases significantly with time on treatment (P = 0.0002 using one-way analysis of variance). Mean expression at 9, 12 and > 14 months is significantly higher than at baseline, as assessed by Dunnett's multiple comparisons test. Data shown represent inverse relative expression. P < 0.05 was considered statistically significant.
Changes in SOCS3 gene expression with time on lenalidomide plus prednisone treatment. Expression of SOCS3 increases significantly with time on treatment (P = 0.0002 using one-way analysis of variance). Mean expression at 9, 12 and > 14 months is significantly higher than at baseline, as assessed by Dunnett's multiple comparisons test. Data shown represent inverse relative expression. P < 0.05 was considered statistically significant.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal