Abstract
Background
The International Prognostic Index (IPI) has been useful prognostic tool to predict prognosis of aggressive non-Hodgkin lymphoma in the last 20 years. Since the advent of R-CHOP (rituximab, cyclophosphamide, doxorubicin, vincristine, and prednisone) chemotherapy for diffuse large B-cell lymphoma (DLBCL), its utility has been challenged and other prognostic index including revised IPI and National Comprehensive Cancer Network (NCCN)-IPI were proposed, which are not popularly used yet. We aimed to develop new prognostic model for DLBCL in rituximab era.
Method
Between March 2004 and June 2012, patients with DLBCL treated with R-CHOP were identified in the database of the Asan Medical Center (AMC) Lymphoma Registry. Primary end point was to devise a new prognostic index for DLBCL. Secondary end point was to validate the NCCN-IPI in our cohort. We tested new prognostic index model in the training set of AMC cohort consisted of randomly selected 80% of the sample (503 patients). The remaining 20% (118 patients) was used as an internal validations set.
Results
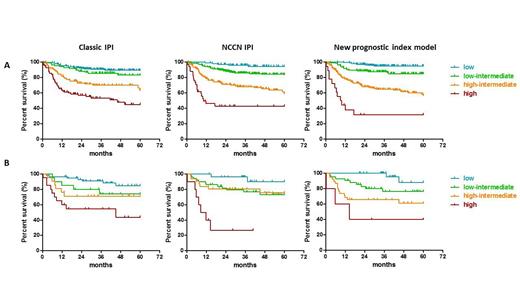
The AMC cohort consisted of 621 patients. Median follow-up duration was 43.3 months (6.2-122.5 months). Baseline characteristics of AMC cohort are presented in table 1. Median age was 57 years (range, 16-85 years). Median ϐ-2 microglobulin (ϐ-2 MG) was 2.10 mg/L (range, 1.0-66.0 mg/L). The univariate analysis of baseline characteristics revealed that age (≦60 vs. >60 years), LDH (within normal vs. increased), ECOG performance (0 or 1 vs. ≧2), advanced stage (Ann Arbor stage I/II vs. III/IV), extra-nodal involvement (≦1 vs. >1), B symptoms (no vs. yes), and ϐ-2 MG (≦2.5 vs. >2.5) could predict overall survival (OS), whereas bulky disease and gender did not (p value 0.140, 0.621, respectively). In the multivariate analysis, age, LDH, ECOG performance status, and ϐ-2 MG were significantly associated with OS (p value 0.001, <0.001, 0.004, and 0.019, respectively), while stage, extra-nodal involvement, and B symptom did not (p value 0.057, 0.233, and 0.577, respectively). We developed a new prognostic model with these 4 significant factors in the multivariate analysis. One point is assigned for each of the risk factors without refined categorization. Four risk groups were composed as followings: low (0 point), low-intermediate (1 point), high-intermediate (2-3 points), and high (4 points). The new prognostic model showed better discriminative power compared with classic IPI (Figure 1A). Five-year OS of low- and high-risk subgroup in new scoring model and classic IPI model in AMC cohort were 95% and 32% versus 89% and 45%, respectively. Our model was validated in an internal validation set (Figure 1B). NCCN-IPI also could stratify four risk groups (Figure 1 A and B).
Conclusion
We propose a new prognostic index model for DLBCL in rituximab era with age, LDH, ECOG performance and ϐ-2 MG, which has good discriminative power and convenient to apply. It warrants further validation using an independent cohort.
Baseline Characteristics
| Characteristics . | Total N=621 % . | Training set N=503 % . | Validation set N=118 % . | |||
|---|---|---|---|---|---|---|
| Age, years Median, range ≦ 60 years > 60 years | 57.0 377 244 | 16-85 60.7 39.3 | 57.0 300 203 | 16-84 59.6 40.4 | 57.0 77 41 | 17-85 65.3 34.7 |
| Sex Male Female | 343 278 | 55.2 44.8 | 273 230 | 54.3 45.7 | 70 48 | 59.3 40.7 |
| ECOG PS 0 or 1 ≧ 2 | 569 52 | 91.6 8.4 | 462 41 | 91.8 8.2 | 107 11 | 90.7 9.3 |
| Serum lactate dehydrogenase levels Normal Elevated | 334 287 | 53.8 46.2 | 279 224 | 55.5 44.4 | 55 63 | 46.6 53.4 |
| Ann Arbor stage I and II III and IV | 293 328 | 47.2 52.8 | 236 267 | 46.9 53.1 | 57 61 | 48.3 51.7 |
| Number of extranodal sites <2 ≧ 2 | 403 218 | 64.9 35.1 | 329 174 | 65.4 34.6 | 74 44 | 62.7 37.3 |
| B symptoms No Yes | 549 72 | 88.4 11.6 | 447 56 | 88.9 11.1 | 102 16 | 86.4 13.6 |
| International prognostic index Low/ low-intermediate High-intermediate/high | 404 217 | 65.1 34.9 | 327 176 | 65.0 35.0 | 77 41 | 65.3 34.7 |
| ¥Â -2 microglobulin, mg/L Median, range ≦ 2.5 mg/L > 2.5 mg/L | 2.1 422 199 | 1.0-66.0 68.0 32.0 | 2.1 339 164 | 1.0-29.6 67.4 32.6 | 2.1 83 35 | 1.0-66.0 70.3 28.7 |
| Characteristics . | Total N=621 % . | Training set N=503 % . | Validation set N=118 % . | |||
|---|---|---|---|---|---|---|
| Age, years Median, range ≦ 60 years > 60 years | 57.0 377 244 | 16-85 60.7 39.3 | 57.0 300 203 | 16-84 59.6 40.4 | 57.0 77 41 | 17-85 65.3 34.7 |
| Sex Male Female | 343 278 | 55.2 44.8 | 273 230 | 54.3 45.7 | 70 48 | 59.3 40.7 |
| ECOG PS 0 or 1 ≧ 2 | 569 52 | 91.6 8.4 | 462 41 | 91.8 8.2 | 107 11 | 90.7 9.3 |
| Serum lactate dehydrogenase levels Normal Elevated | 334 287 | 53.8 46.2 | 279 224 | 55.5 44.4 | 55 63 | 46.6 53.4 |
| Ann Arbor stage I and II III and IV | 293 328 | 47.2 52.8 | 236 267 | 46.9 53.1 | 57 61 | 48.3 51.7 |
| Number of extranodal sites <2 ≧ 2 | 403 218 | 64.9 35.1 | 329 174 | 65.4 34.6 | 74 44 | 62.7 37.3 |
| B symptoms No Yes | 549 72 | 88.4 11.6 | 447 56 | 88.9 11.1 | 102 16 | 86.4 13.6 |
| International prognostic index Low/ low-intermediate High-intermediate/high | 404 217 | 65.1 34.9 | 327 176 | 65.0 35.0 | 77 41 | 65.3 34.7 |
| ¥Â -2 microglobulin, mg/L Median, range ≦ 2.5 mg/L > 2.5 mg/L | 2.1 422 199 | 1.0-66.0 68.0 32.0 | 2.1 339 164 | 1.0-29.6 67.4 32.6 | 2.1 83 35 | 1.0-66.0 70.3 28.7 |
Multivariate Analysis for Factors Associated with Overall Survival
| Factors . | HR . | 95% CI . | P value . | Score . |
|---|---|---|---|---|
| Age, years ≦ 60 years > 60 years | 1.000 2.051 | 1.362-3.090 | 0.001 | 1 |
| Serum lactate dehydrogenase levels Normal Elevated | 1.000 3.165 | 1.951-5.135 | <0.001 | 1 |
| ECOG PS 0 or 1 ≧ 2 | 1.000 2.073 | 1.261-3.407 | 0.004 | 1 |
| ϐ -2 microglobulin, mg/L ≦ 2.5 mg/L > 2.5 mg/L | 1.000 1.691 | 1.0391-2.622 | 0.019 | 1 |
| Factors . | HR . | 95% CI . | P value . | Score . |
|---|---|---|---|---|
| Age, years ≦ 60 years > 60 years | 1.000 2.051 | 1.362-3.090 | 0.001 | 1 |
| Serum lactate dehydrogenase levels Normal Elevated | 1.000 3.165 | 1.951-5.135 | <0.001 | 1 |
| ECOG PS 0 or 1 ≧ 2 | 1.000 2.073 | 1.261-3.407 | 0.004 | 1 |
| ϐ -2 microglobulin, mg/L ≦ 2.5 mg/L > 2.5 mg/L | 1.000 1.691 | 1.0391-2.622 | 0.019 | 1 |
IPI versus NCCN IPI versus new prognostic index model in Asan Medical Center training set (A) and internal validation set (B)
IPI versus NCCN IPI versus new prognostic index model in Asan Medical Center training set (A) and internal validation set (B)
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal