Abstract
The addition of rituximab to CHOP (R-CHOP; CHOP, cyclophosphamide, doxorubicin, vincristine, and prednisolone) has significantly improved the outcome of diffuse large B-cell lymphoma (DLBCL). However, its secondary involvement in the central nervous system (CNS) is still a fatal event, and optimal therapeutic strategies have remained to be established. Combined immunochemotherapy with rituximab, methotrexate, procarbazine, and vincristine (R-MPV) followed by consolidation reduced-dose whole-brain radiotherapy and high-dose cytarabine is currently in use for patients with CNS relapse, though treatment outcome has not been evaluated enough. In the present study, we aimed to analyze the incidence and prognosis of CNS relapse of aggressive B-cell lymphoma in comparison with those of systemic relapse in the era of rituximab-containing regimens. We also estimated the risk factors and prognostic factors for CNS relapse.
We retrospectively analyzed 278 consecutive adult patients (≥16 years old) who were diagnosed as DLBCL or primary mediastinal large B-cell lymphoma (PMLBL) at The University of Tokyo Hospital, Tokyo, Japan, from August 2003 through August 2013. We excluded patients who had CNS or intraocular involvement at diagnosis since those patients had received high-dose methotrexate-based therapy instead of R-CHOP. Four to six courses of intrathecal administration of methotrexate were performed in patients with adrenal gland, testis or breast involvement as prophylaxis for CNS relapse.
The median follow-up period was 42 months, and the median age was 66 years (range, 23-91). Overall, 67 patients (24.1%) had relapse at any site, of which 24 patients (35.8%) had CNS involvement. The median interval between initial diagnosis and the occurrence of secondary CNS involvement was 212 days, and 15 of the 24 patients (62.5%) had CNS relapse within 1 year from the initial diagnosis. Multivariate analysis revealed that multiple or diffuse extranodal involvement at initial diagnosis (hazard ratio [HR] 3.74, 95% confidence interval [CI] 1.28-10.91; P<0.01) was associated with the development of CNS relapse against non-CNS relapse. Chromosomal abnormality was investigated in 112 patients, of which 38 had abnormal karyotypes as identified by G-banding analysis for lymph nodes. Patients with CNS relapse more frequently harbored chromosomal abnormalities compared with those without relapse in univariate analysis (P=0.01).
We also analyzed the survival of patients with primary CNS lymphoma (PCNSL) as a control. Only two (7%) of 27 patients with PCNSL died during the follow-up period. Five-year OS from initial diagnosis was 92.3% (95% CI: 82.5-100.0%), and was significantly better than that for patients with CNS relapse (33.9%, 95% CI: 17.3-66.3%, P<0.01).
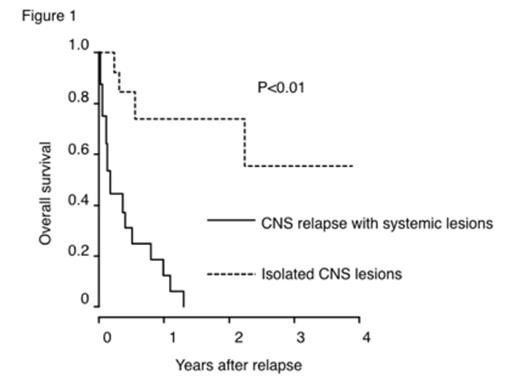
Among 24 patients with CNS relapse, eight (33%) had systemic lesions other than CNS when diagnosed as CNS relapse, and four (17%) patients newly developed systemic lesions while treated for CNS relapse. Patients without concurrent systemic lesions attained a rather good prognosis by chemo-radiotherapy, while those harboring concurrent systemic lesions had dismal outcome (one-year OS after the diagnosis of relapse: 74.0% versus 12.4%, P<0.01, Figure 1, systemic relapse was treated as a time-dependent covariate).
These results indicate that controlling systemic lesions as well as CNS ones is essential for treating patients with secondary CNS involvement of DLBCL. CNS lesions would be well controlled with R-MPV implementation as salvage therapy, nevertheless we should be careful for concurrent systemic lesions which might require different therapeutic strategies.
Nannya:Chugai Pharmaceutical CO., LTD: Speakers Bureau; Pfizer: Research Funding. Kurokawa:Chugai Pharmaceutical CO., LTD: Research Funding, Speakers Bureau; Pfizer Japan Inc.: Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal