Abstract
Abstract
Background: CNS relapse is uncommon but challenging complication in patients with mantle cell lymphoma (MCL). Survival after CNS relapse is extremely poor that identification of high risk population is therefore critical in whom prophylactic chemotherapy may play a role.
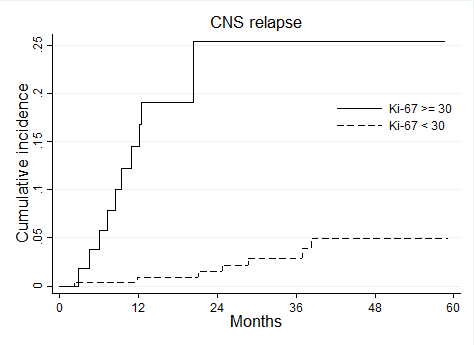
Patients and Methods: A total of 405 patients (median age, 66 years; range 22-85) with MCL newly diagnosed between 1994 and 2012 at 48 institutions in Japan were analyzed.Pathological specimens were centrally reviewed in all patients. We evaluated risk factors for CNS relapse in patients with MCL using competing risk regression analysis. Patients were excluded if they had evidences of CNS involvement at initial diagnosis. Overall, 81% of the patients received rituximab containing regimen with 222 patients received CHOP, 133 patients received high-dose cytarabine containing regimen and 50 patients received other regimen such as fludarabine. At a median follow up duration of 40.4 months, 25 patients (6.2%) experienced CNS relapse. Five patients presented with brain parenchymal mass, 13 patients presented with leptomeningeal disease, and 7 patients presented with both. The median time from initial diagnosis to CNS relapse was 18.5 months. Two-year cumulative incidence of CNS relapse was 4.7% (95%CI: 2.8-7.3). No difference was seen in the incidence of CNS relapse between the treatment with or without rituximab. Univariate analysis revealed blastoid or pleomoriphic variant, Ki-67 ≥ 30, serum total protein < 6.0g/dl, leukemic presentation and high risk group in simplified-MIPI at diagnosis as significant risk factors for CNS relapse. Within these five factors, Ki-67 was the strongest predictive factor for CNS relapse with hazard ration of 8.7 (95%CI: 3.4-22.2). Two-year cumulative incidence of CNS relapse in patients with Ki-67 ≥ 30 was 25.4% (95%CI: 13.5-39.1), while that in patients with Ki-67 < 30 was 1.5% (95%CI: 0.2-2.9) (Figure). Ki-67 ≥ 30 was a significant risk factor for CNS relapse both in patients who received CHOP and hyper-CVAD/MA. Survival after CNS relapse was dismal with median survival time of 5.7 months.
Summary: We identified four risk factors for CNS relapse in patients with MCL. Within these factors, Ki-67 ≥ 30 is the strongest predictive factor with 2-year cumulative incidence of 25.4%. Evaluation for CNS involvement at the diagnosis and assessment for value of prophylactic IT chemotherapy is mandatory in patients with Ki-67 ≥ 30.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal