Abstract
INTRODUCTION
CNS relapse in DLBCL carries poor prognosis. Some studies have suggested decreased incidence with rituximab, but there are several others reporting otherwise. We analyzed prospective studies in literature to understand the role of rituximab and CNS prophylaxis in DLBCL, in comparison to CHOP based therapy.
METHOD
Extensive searches using PUBMED, EMBASE, CENTRAL and major hematology conferences were conducted for prospective studies. The keywords CNS, diffuse large B-cell lymphoma, relapse, prophylaxis, rituximab, CHOP were used. Inclusion: (i) prospective or randomized trials (ii) Entire study population or a significant majority of patients were newly diagnosed DLBCL, (iii) no evidence of CNS involvement at baseline, (iv) use of rituximab-chemotherapy or CHOP-based chemotherapy, (v) have data relevant to our study. Exclusion: (i) retrospective studies, review article or case reports, (ii) exclusively testicular, mediastinal or double hit lymphoma, (iii) HIV positive patients. Data is presented as mean ± standard error of mean. Significant differences (at P<0.05) between groups and couplets were determined by one-way ANOVA and by two-tailed unpaired t-test respectively. Significance of the Kaplan-Meier survival curves was determined using Log-rank (Mantel-Cox) and Gehan-Breslow-Wilcoxon tests.
RESULTS
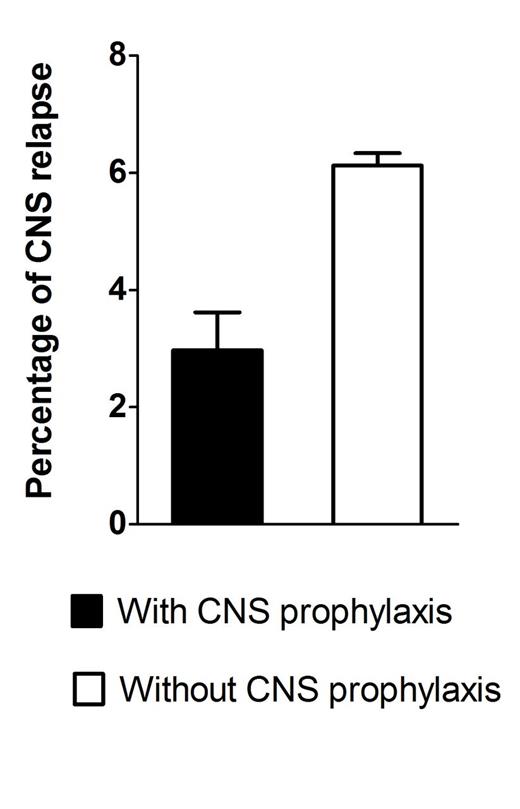
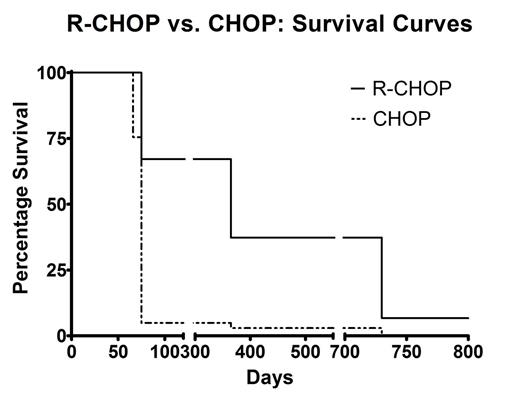
The study population characteristics are shown in Table. The mean incidence of CNS relapse with rituximab-chemotherapy (R-CHOP/R-CHOEP) was found to be 5.52% (3.21%-7.73%), while that with CHOP-based chemotherapy alone was 4.43% (3.53% -5.33%). No significant difference was observed by two-tailed unpaired t test (P = 0.94). The median time from diagnosis to CNS relapse was 6.5-7 months. The mean incidence of leptomeningeal, parenchymal and both relapses in the rituximab-chemotherapy group were 38.62(±1.93)%, 57.32(±3.06)%, 5.36(±1.79)% compared to 16.17(±0.44)%, 66.17(±0.44)%, 22.06(±0.41)% with chemotherapy alone. One-way ANOVA also showed that use of rituximab resulted in statistically significant (P<0.0001) differences between the patterns of CNS relapse. About 74.1% of CNS relapses among patients receiving rituximab-chemotherapy were isolated CNS relapse, compared to 69.2% for those receiving CHOP chemotherapy. The mean incidence of CNS relapse with the use of any prophylactic CNS directed therapy was observed to be a significantly (P = 0.044) lower [2.97% (2.32%-3.62%)] compared to that without [6.12% (5.91%-6.335]. Median survival following CNS relapse of 365 days following rituximab based chemotherapy and 75 days after CHOP were significantly different (HR for CHOP use 4.867±0.77 at P<0.05).
CONCLUSION
Rituximab hasn't significantly decreased overall incidence, but causes less parenchymal CNS relapse. CNS prophylaxis has a definite role in high risk population. There is significantly better survival after CNS relapse in the rituximab era.
| STUDY . | Age (yr) . | Sex (M:F) . | No. . | Stage 3/4 . | IPI int-high/ high (>=3 IPI or >=2 aa IPI) . | Extranodal (>=2) . | high LDH . | Follow up (m) . | Criteria for CNS prophylaxis . | Patients receiving CNS prophylaxis (IT=intrathecal,S=systemic) . | Chemo . |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Tilly 2003 | 61-69 | ACVBP vs CHOP : M 182 vs 177 F 141 vs 135 | 635 (501 DLBCL) | 267 vs 253 | 210 vs 207 (aa IPI) | 155 VS 156 | 231 VS 241 | 68 | None for CHOP VS ACVBP (IV methotrexate, etop + IT mtx) | 323 (ACVBP) | 323 ACVBP vs 312 CHOP |
| Feugier 2004 | 69 | M 92 (CHOP-R) vs 107 (CHOP) | 202 vs 197 | 161 vs 157 | 121 vs 120 | 61 vs 51 | 131 vs 132 | 24 | NA | no prophylaxis | 202 R-CHOP Vs 197 CHOP |
| Bernstein 2009 | 97/ 225 for CHOP were >60 yrs | NR | 899 aggressive lymphoma | 191/ 225 CHOP | 95/ 225 CHOP | 81/225 CHOP | 146/ 225 CHOP | 20 years | none for CHOP | 121 IT MTX or radiation (24 Gy) | 225 CHOP vs ProMACE-CytaBOM vs mBACOD vs MACOP-B |
| Boehme 2009 | 68 | 648 vs 569 | 1217 (944 DLBCL) | 687 | 507 | 212 | 602 | 24 | bone marrow, testes, sinuses, orbits, oral cavity, tongue, salivary glands. | 475/1217 (IT-MTX) | 608 RCHOP Vs 609 CHOP |
| Kim 2012 | 59.5 | NR | 564 | 276 | 192 | 193 | NR | 10.5 | ≥1 risk factor | 59 IT | RCHOP |
| Kumar 2012 | 56 (prophylaxis) VS 58 (no prophylaxis) | male: 74 vs 476 female: 43 vs 396 | 989 | 85 vs 454 | 55 vs 240 | 66 vs 220 | 57 vs 372 | 30 | High risk site involvement : orbit, testis, peripheral blood, vertebra, bone marrow, nasal/paranasal sinuses | 117/989 IT- 84/117 (AraC/MTX) S--33/117 (MTX) | R-CHOP |
| Holte 2013 | 54 | 97 vs 59 | 156 (145 DLBCL) | 150 | 156 | 41 | 151 | 36 | everyone | 156/156 (S- Ara-c+ MTX) 1 dose of IT-MTX | RCHOEP |
| STUDY . | Age (yr) . | Sex (M:F) . | No. . | Stage 3/4 . | IPI int-high/ high (>=3 IPI or >=2 aa IPI) . | Extranodal (>=2) . | high LDH . | Follow up (m) . | Criteria for CNS prophylaxis . | Patients receiving CNS prophylaxis (IT=intrathecal,S=systemic) . | Chemo . |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Tilly 2003 | 61-69 | ACVBP vs CHOP : M 182 vs 177 F 141 vs 135 | 635 (501 DLBCL) | 267 vs 253 | 210 vs 207 (aa IPI) | 155 VS 156 | 231 VS 241 | 68 | None for CHOP VS ACVBP (IV methotrexate, etop + IT mtx) | 323 (ACVBP) | 323 ACVBP vs 312 CHOP |
| Feugier 2004 | 69 | M 92 (CHOP-R) vs 107 (CHOP) | 202 vs 197 | 161 vs 157 | 121 vs 120 | 61 vs 51 | 131 vs 132 | 24 | NA | no prophylaxis | 202 R-CHOP Vs 197 CHOP |
| Bernstein 2009 | 97/ 225 for CHOP were >60 yrs | NR | 899 aggressive lymphoma | 191/ 225 CHOP | 95/ 225 CHOP | 81/225 CHOP | 146/ 225 CHOP | 20 years | none for CHOP | 121 IT MTX or radiation (24 Gy) | 225 CHOP vs ProMACE-CytaBOM vs mBACOD vs MACOP-B |
| Boehme 2009 | 68 | 648 vs 569 | 1217 (944 DLBCL) | 687 | 507 | 212 | 602 | 24 | bone marrow, testes, sinuses, orbits, oral cavity, tongue, salivary glands. | 475/1217 (IT-MTX) | 608 RCHOP Vs 609 CHOP |
| Kim 2012 | 59.5 | NR | 564 | 276 | 192 | 193 | NR | 10.5 | ≥1 risk factor | 59 IT | RCHOP |
| Kumar 2012 | 56 (prophylaxis) VS 58 (no prophylaxis) | male: 74 vs 476 female: 43 vs 396 | 989 | 85 vs 454 | 55 vs 240 | 66 vs 220 | 57 vs 372 | 30 | High risk site involvement : orbit, testis, peripheral blood, vertebra, bone marrow, nasal/paranasal sinuses | 117/989 IT- 84/117 (AraC/MTX) S--33/117 (MTX) | R-CHOP |
| Holte 2013 | 54 | 97 vs 59 | 156 (145 DLBCL) | 150 | 156 | 41 | 151 | 36 | everyone | 156/156 (S- Ara-c+ MTX) 1 dose of IT-MTX | RCHOEP |
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal