Abstract
Background: Cutaneous T cell lymphoma (CTCL) is a rare/orphan disease. Mycosis fungoides (MF) and Sézary syndrome (SS) are the major subtypes. Most patients with MF present in early stages (IA-IIA) with a good prognosis. However a third present in advanced stages (IIB-IVB) with a median survival of 1-5yrs. Clinical management is stage-based; however there is wide range of outcome within clinical stages. Currently, we lack evidence based prognostic information for further stratification that can optimize clinical management or be applied in therapeutic trials. Published prognostic studies in MF/SS have largely been single centre. A retrospective study from the UK & a US site proposed a potential prognostic model for MF/SS (Benton et al Eur J Cancer 2013;49:2859-68) but is limited in power and lacking standardised definitions. Due to the small numbers of patients presenting with advanced stage disease only a large collaboration would power a study to determine prognostic parameters with international relevance. Towards this aim, we have established an international collaborative alliance, the Cutaneous Lymphoma International Consortium (CLIC), to acts as an efficient conduit where well-defined parameters and end-points are used to design studies. This retrospective CLIC study tests selected prognostic parameters against survival in advanced stages of MF/SS in order to determine power and identify prognostic markers that impact globally and may be used in future prospective studies to establish an international prognostic index.
Methods: We reviewed the literature of prognostic markers in MF/SS and identified 11 candidate clinical, pathological, and laboratory parameters; 1) stage, 2) age, 3) male sex, 4) modified skin weighted assessment tool score (MSWAT), histological features of 5) folliculotropism, 6) CD30 positivity, 7) proliferation index (%Ki-67 staining) & 8) large cell transformation(LCT), 9) leucocyte/lymphocyte count, 10) LDH & 11) identical T-cell clone in blood & skin. Data were collected on patients presenting with advanced stages of MF/SS (IIB-IVB) diagnosed after the new staging system [Olsen et al. Blood. 2007;110:1713-22].
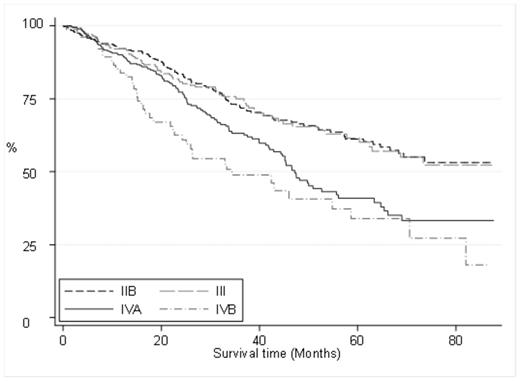
Results: Twenty-five international sites (16 EU, 6 US, 1 Australian, 1 Asian, 1 South American) identified 1249 MF/SS patients presenting with advanced stage disease since 2007. Patients with complete staging and outcome data (91% 1147 patients) were included in the analyses. MSWAT was not tested due to incompleteness of data (26%). Data completeness for the other 9 prognostic variables ranged from 38-100%. Median survival for this advanced stage cohort was 65 months with 2 and 5 year survival of 79% and 53%, respectively. The median survival for Stage IIB and III was not reached (restricted mean survival was 63 months in both stage IIB & III), median survival for stage IVA was 47 months and 44 months in stage IVB (Fig 1). In univariate analysis 4/9 variables were significantly associated with decreased survival including age>60 years (data 100% complete, p<0.001), LCT in skin (data 87% complete, p=0.007), elevated LDH (data 71% complete, p<0.001) and raised leucocytes (data 68% complete, p=0.004). In multivariate analysis including these 4 variables only age >60 (p=0.08) and LDH (p=0.008) were significant. According to stage; age>60, LDH & LCT were associated with a worse survival in stage IIB, in stage III only age & LDH and in stage IVA LDH & a raised leucocyte count were significant.
Conclusion: This study has proven the ability of the CLIC to work cohesively, as the first large-scale international collaboration in CTCL. The current staging system shows similar survival in stage IIB and III disease (Fig 1) highlighting the need for further refinement within these stages. Our analysis found age>60yrs & LDH are independent prognostic parameters with potential relevance in advanced stages of MF/SS. This study has highlighted the need for prospective data collection due the intrinsic flaws of retrospective analysis including missing data, lack of standard definitions rendering some data unusable and potential bias in more complete data in aggressive subtypes. Future prospective studies with well-defined criteria and more complete data collection will be required to better identify parameters of prognostic significance and to test their utility towards building a prognostic index model.
Kaplan Meier Survival Curves According to Stage
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal