Abstract
Background: The incidence of venous thromboembolism (VTE) is rising in critically ill children. It is one of the most common hospital acquired complications and the use of thromboprophylaxis remains controversial. Exposure to risk factors including central venous lines, infection/inflammation and prolonged immobilization increases the risk of VTE while underlying coagulopathy, thrombocytopenia, requirement of invasive procedures, organ failure or medications increase the risk of bleeding. Therefore, understanding these risk factors in various subsets of critically ill children is vital to develop VTE prevention strategies. Since Hematopoietic Stem Cell Transplant (HSCT) recipients comprise a subset of patients at high risk of developing VTE due to exposure to the risk factors above, we explored the trends and risk factors for VTE in children undergoing HSCT using a national administrative database during the past decade.
Methods: ThePediatric Health Information System (PHIS) database was queried using the ICD-9-CM codes to identify children <=18 years old who underwent HSCT at 40 hospitals from 2004-2013. A step-wise search strategy was developed to identify the subset of patients whose billing codes indicate that they had developed at least one incidence of VTE after discharge or during their HSCT admission. The patient level data (age, gender, ethnicity, pre-HSCT diagnosis) and HSCT related data [Graft versus host disease (GVHD), Veno-occlusive disease (VOD), Cytomegalovirus infection (CMV) and length of stay) was abstracted from the HSCT encounter. Descriptive analyses were performed to compare means, and percentages between VTE and various risk factors. Chi Square and Fisher exact test were used as appropriate. We performed a linear regression analysis to compare the trends of VTE over the last 10 years.
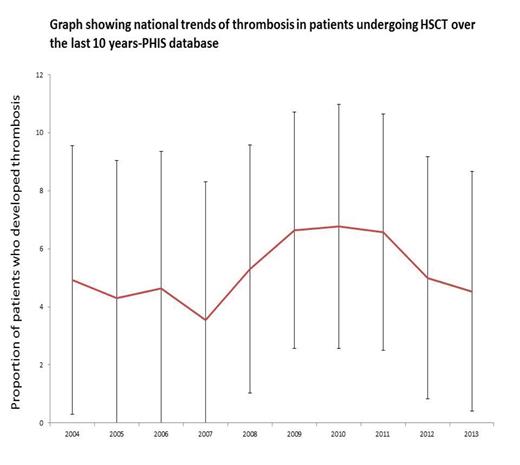
Results: A total of 8559 children underwent HSCT from 2004 to 2013. Of these, 450 (5.26%) developed VTE after HSCT discharge. The details of patient characteristics are shown in Table 1. The VTE incidence and 95% confidence intervals by year are shown in figure 1. There was no significant linear change in the trends of VTE in the patients undergoing an HSCT over the last 10 years, (p=0.296), Figure 1. In bivariate analyses, patients who developed VTE were older, had more hematological malignancies, longer length of hospitalization during the encounter and had higher incidence of acute GVHD (aGVHD), chronic GVHD (cGVHD) and VOD (p<0.001).
Conclusions: This study showed that despite concerns about rising incidence of VTE in critically ill hospitalized children, the incidence of VTE as defined by the billing codes in the HSCT population has remained stable during the last decade.We have also described that age, prolonged hospitalization and hematological malignancy were associated with occurrence of VTE in this group of patients. The higher incidence of aGVHD, VOD and cGVHD in patients imply that ongoing inflammation predisposes to prothrombotic milieu. These findings warrant consideration prior to implementing VTE prophylaxis in HSCT patients. More prospective studies are needed to explore the utility of primary thromboprophylaxis in this population.
| Characteristic . | Patients with thrombosis N=450 . | Patients without thrombosis N=8109 . | p-value . |
|---|---|---|---|
| Age (years) Mean St. Deviation | 9.2 5.9 | 8 5.3 | <0.0001 |
| Gender Male Female | 249 (55%) 201 (45%) | 4717 (58%) 3392 (42%) | 0.235 |
| Ethnicity Hispanic Non-hispanic Unknown | 79 (18%) 221 (49%) 150 (33%) | 1546 (19%) 3593 (44%) 2970 (37%) | 0.136 |
| Diagnosis Aplastic anemia Hematological malignancy (including MDS) NHL Brain tumor SCID Sickle Cell Disease Thalassemia Others | 24 (5%) 158 (35%) 19 (4%) 23 (5%) 11 (2%) 7 (2%) 0 (0%) 208 (46%) | 498 (6%) 2412 (30%) 213 (3%) 554 (7%) 166 (2%) 131 (2%) 2 (0.02%) 4133 (51%) | 0.485 0.017 0.042 0.156 0.564 0.921 0.739 |
| Length of stay (days) Mean St. Deviation | 59 51.91 | 44 34.06 | <0.0001 |
| Acute GVHD | 75 (17%) | 729 (9%) | <0.0001 |
| Chronic GVHD | 73 (16%) | 521 (6%) | <0.0001 |
| VOD | 14 (3%) | 124 (2%) | 0.009 |
| CMV Viremia | 15 (3%) | 236 (3%) | 0.604 |
| Characteristic . | Patients with thrombosis N=450 . | Patients without thrombosis N=8109 . | p-value . |
|---|---|---|---|
| Age (years) Mean St. Deviation | 9.2 5.9 | 8 5.3 | <0.0001 |
| Gender Male Female | 249 (55%) 201 (45%) | 4717 (58%) 3392 (42%) | 0.235 |
| Ethnicity Hispanic Non-hispanic Unknown | 79 (18%) 221 (49%) 150 (33%) | 1546 (19%) 3593 (44%) 2970 (37%) | 0.136 |
| Diagnosis Aplastic anemia Hematological malignancy (including MDS) NHL Brain tumor SCID Sickle Cell Disease Thalassemia Others | 24 (5%) 158 (35%) 19 (4%) 23 (5%) 11 (2%) 7 (2%) 0 (0%) 208 (46%) | 498 (6%) 2412 (30%) 213 (3%) 554 (7%) 166 (2%) 131 (2%) 2 (0.02%) 4133 (51%) | 0.485 0.017 0.042 0.156 0.564 0.921 0.739 |
| Length of stay (days) Mean St. Deviation | 59 51.91 | 44 34.06 | <0.0001 |
| Acute GVHD | 75 (17%) | 729 (9%) | <0.0001 |
| Chronic GVHD | 73 (16%) | 521 (6%) | <0.0001 |
| VOD | 14 (3%) | 124 (2%) | 0.009 |
| CMV Viremia | 15 (3%) | 236 (3%) | 0.604 |
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal