Abstract
Background:
Within the Haematology and Oncology department at a London Teaching Hospital Peripherally Inserted Central Catheters (PICC) are inserted by the Nurse Practitioners (NP) and tip position is checked by radiological confirmation post procedure. Inpatients were found to be waiting on average 5 hours for a chest xray (CXR), delaying therapies. Confirming tip position post insertion also led to repeat procedures if the tip was found to be malpositioned on the CXR film.
Introduction:
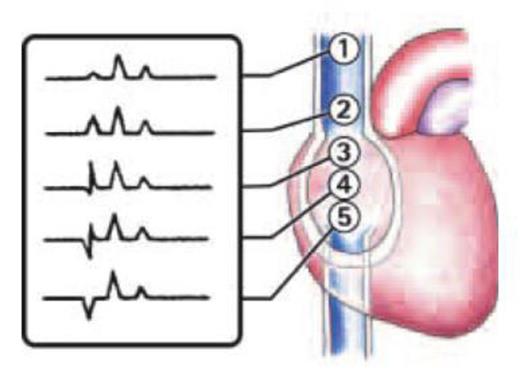
ECG can be used to verify tip positions of central venous catheters. The technique was first introduced in the 1940s in Europe but the potential was not realised until 50 years later. The practice works by attaching the patient to a cardiac monitor, and connecting an extra lead to the PICC. Pulses from the Sinoatrial Node are detected by the PICC as it enters the Superior Vena Cava. The impulse grows stronger as the tip advances down the vein, signified by an enlarged p-wave visible on the ECG. Passing the node causes a deflection in the wave, communicating to the inserter that the tip is positioned beyond the Cava-Atrial Junction (CAJ) i.e. into the right atrium, and should be retracted. The ideal tip position for a PICC line is between the distal SVC and within one centimetre of the right atrium. This method of insertion is not suitable for all patient groups. It is well documented that obese, the young or patients with AF will not obtain a clear p-wave rise. Also the presence of a pacemaker will mean that the p-wave size is not affected by the PICC tip position.
Ideal tip position of a PICC line provides reliable venous access with optimal therapeutic delivery, while minimizing short-and-long term complications. Prior to engaging in the data collection, the Nurse Practitioners completed an ECG course, participated in a company workshop and consolidated their training by visiting another trust who were also performing ECG guided PICC insertions.
Method:
A study of 120 patients compromising of 66 females and 54 males from October 2013 – July 2014 was performed. 103 PICC lines were required for chemotherapy treatment, the remaining 17 PICC line were for supportive therapies. 36 PICC lines were inserted on the left side and 84 PICC lines inserted on the right.
PICCs were placed under ECG guidance and a post-procedural CXR was performed. The NP predicted the position of the tip based on the ECG tracing, and comparison was made once the CXR was performed and the radiological report made available.
Results
Out of 120 cases, 10 patients failed to obtain a p-wave rise that the inserter deemed significant. However according to the radiological image all of these lines were found to be suitably positioned. The incidence of this phenomenon was greatly reduced once the practitioners gained experience of this technique. There was one case where the p-wave rise was deemed significantly high by both practitioners to predict a positioning of the CAJ. However following a CXR, the line was incorrectly positioned at the top of the SVC. This was of concern; however the patient was a complex case, with Budd-Chiari syndrome, causing abdominal distension and compression of the organs. In published literature, below diaphragm abnormalities can impact on the sensitivity of the technique. For this reason complicated patients, such as described will require consideration of radiological imaging.
In all other cases where the P wave was appropriately elevated the chest radiograph image that followed demonstrated a definite correlation between the height (size) of the P-wave and the location of the terminal tip is within the SVC.
Conclusion
The data significantly supported ECG guidance as an accurate verification for PICC tip position. Currently the department is planning on foregoing the post-insertion CXR if the ECG method has produced a positive result. The Nurse Practitioners recognise that there will always be cases that require a CXR. However use of the ECG method will reduce the time between insertion and use of the PICC line, diminish radiation exposure to our patients and lower the costs of repeated insertion due to malpositioning of lines.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal