Abstract
Background: Outcomes in multiple myeloma (MM) have significantly improved, leading to higher prevalence of this disease. Increasing efforts have been made by various agencies to educate patients (pts), manage quality of life (QoL) and survivorship. A global impact of these efforts including pt awareness, disease knowledge and participation in their care, as well as the physical and emotional impact of MM and its treatments (Rx) has not been assessed. We undertook an international, pt-reported survey to investigate these factors and understand any underlying disparities.
Methods: A 61-question patient-reported questionnaire (MM-Q), addressing global aspects of MM pts care (components in Figure 1) was used. MM-Q was administered in collaboration with the International Myeloma Foundation (IMF). To limit responses by MM pt only, SmartPatient MM community members and IMF Support Group Leader list were invited to complete the survey. Some of the questions were mandatory, and those with missing responses were withdrawn from the final analysis of that pts MM-Q. Categorical and continuous variables were compared among groups using the Chi-square and Kruskal-Wallis tests, respectively using SAS software (v9.3) with a two-sided significance level of 0.05.
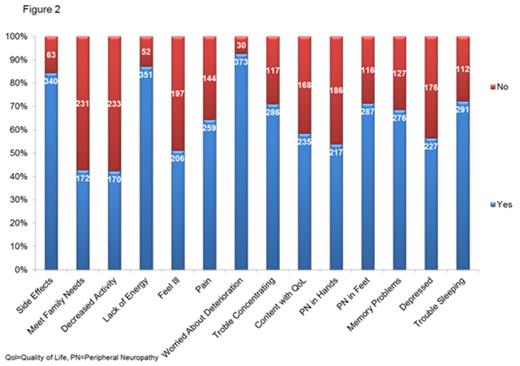
Results: Survey responses are available from 894/1240 (72%) individuals thus far. Average survey completion time was 16 minutes. Data from 746 MM-Q was included in this analysis with 466 (62.5%) complete responses. Pts from United States (US) represented 85.7% of the responders (majority from New York State). Ethnicity (n=590) was reported as non-Latino by 97%, race (n=580) was reported as White by 95%, family history of MM was reported by 19 pts and 81 reported prior history of a primary malignancy (most common, 37% non-melanoma skin cancer). Living situation questions (n=538) revealed majority were in a household of 2 (62%), were unemployed/on public assistance (53.5%), travelled alone to medical appointments (74%), with travel times varying from <30 min (55%) to >1 hr (17%). Majority (83%) had no prior knowledge of MM, 63% were patient support group members, and 92% did MM-related research on internet. With respect to MM Rx (n=524), 70% had been on Rx within 3 months and 12% reported non-compliance. Prior Rx included thalidomide (30%), lenalidomide (66%), pomalidomide (11.5%), bortezomib (63.5%), carfilzomib (11%), steroids (100%), and clinical trial participation in 25% pts. Side effects from Rx/QoL in prior 3 months (n=403) are summarized in figure 2. Pts satisfaction with Rx/treating staff (n=378) revealed majority felt their Rx to be effective (92%), right for them (87%) and side effects were as expected (84%). In general, pts acknowledged positive attributes of the Rx staff (worked towards same goal; 91%, participated in decisions; 81%, honesty 89%, confidence; 92%), and their doctor's explanations regarding Rx (benefits; 84%, side effects; 74%, test results; 83%), with the exception of emotional effects of Rx (48%). 94% pts rated their care as good/excellent and 95% were willing to participate in a follow-up survey. Stratification of statistically significant responses by geographical categories, age and time since diagnosis are shown in table 1 and analysis by occupation and educational status is ongoing.
Conclusions: We conducted a large patient-reported survey to understand the current state of awareness among MM pts and a global impact of the diagnosis and its Rx on them. We showed that majority of pts who accessed the survey responded (72%), which may be a product of literacy, education and access to technology. Majority of the pts were White and non-Latino, highlighting the possible role of access and awareness in ethnic minorities. We report the large prevalence of psychophysical burden of MM and its Rx in MM pts. In general, MM pts had a high rate of satisfaction related to the Rx and their healthcare providers, but the frequency of discussion regarding emotional effects of Rx between doctors and pts was conspicuously low (48%) and the more recently diagnosed pts were less likely to be satisfied with their treating staff. We also demonstrated significant behavioral pattern differences in geographical, age and time-since-diagnosis subgroups, some of which may be sociocultural, while others may be a result of more patient awareness and understanding of the disease. This knowledge will be very helpful in devising MM survivorship strategies.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.



This feature is available to Subscribers Only
Sign In or Create an Account Close Modal