Abstract
Background: In relapsed or refractory acute myeloid leukemia (AML), long-term disease-free survival may only be achieved with allogeneic hematopoietic stem cell transplantation (HSCT). Within the BRIDGE Trial, the safety and efficacy of a clofarabine salvage therapy as a bridge to HSCT was studied. Here, we report long-term survival data and the impact of donor availability at the time of study enrollment. The BRIDGE trial (NCT 01295307) was a phase II, multicenter, intent-to-transplant study.
Patients and Methods: Between March 2011 and May 2013, 84 patients with relapsed or refractory AML older than 40 years were enrolled. Patients were scheduled for at least one cycle of induction therapy with CLARA (clofarabine 30 mg/m2 and cytarabine 1 g/m2, days 1-5). Patients with a donor received HSCT in aplasia after first CLARA. In case of a prolonged donor search, HSCT was performed as soon as possible. The conditioning regimen consisted of clofarabine 30 mg/m2, day -6 to -3, and melphalan 140 mg/m2 on day -2. In patients with partially matched unrelated donors, ATG (Genzyme) at a cumulative dose of 4.5 mg/kg was recommended. GvHD prophylaxis consisted of CsA and mycophenolate mofetil.
Results: Forty-four patients suffered from relapsed AML and 40 patients had refractory disease. The median patient age was 61 years (range 40 – 75). According to the current ELN risk stratification 17% of pts were classified as favorable risk, 35% as intermediate I, 17% as intermediate II and 20% as adverse risk.
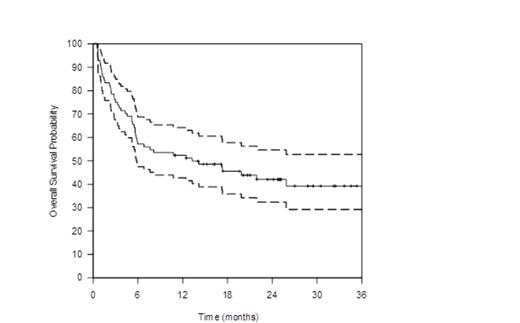
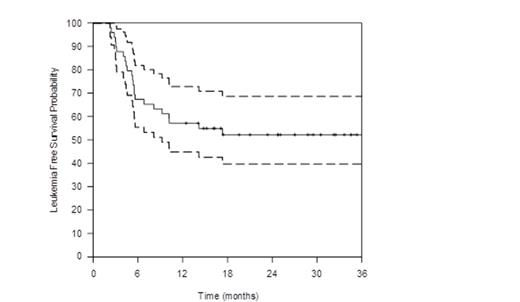
The overall response rate assessed at day 15 after start of CLARA was 80% (defined as at least a marked reduction in BM blasts or BM cellularity and absence of blasts in the peripheral blood) with 31% of patients having less than 5% BM blasts at that time. Seventeen patients did not respond to CLARA, and were subsequently treated off-study. Due to early death, three patients were not evaluable for treatment response. Overall, 66% of the patients received HSCT within the trial. Donors were HLA-identical siblings in eight cases (14%), HLA-compatible unrelated donors in 30 cases (55%) and unrelated donors with one mismatch in 17 cases (31%). Treatment success was defined as complete remission (CR), CR with incomplete recovery (CRi) or CRchim (BM donor chimerism >95% and absolute neutrophil count >0.5/nL) on day 35 after HSCT. Treatment success was achieved in 61% of the patients. With a median follow up of 25 months, the OS for all enrolled patients at two years was 42% (95% CI, 32% to 54%). (Figure 1) The Leukemia-free survival at two years for those 51 patients who achieved the primary endpoint was 52% (95% CI, 40% to 69%). (Figure 2)
At the time of enrollment, 14% of patients had a related donor and 33% had an unrelated donor available. In 46% of the patients, donor search was initiated at the time of enrollment. For 7% of patients, donor search was unsuccessful prior to enrollment and reinitiated. The OS at 2 years for patients with a related or an unrelated donor available was 75% (95% CI, 54% to 100%) and 47% (95% CI, 31% to 71%), respectively, while it was 29% (95% CI, 18% to 48%) for patients for whom donor search was initiated at time of enrollment (p = .09).
Conclusions:
Salvage therapy with CLARA, and subsequent conditioning with clofarabine and melphalan prior to allogeneic HSCT, provides good anti-leukemic activity in patients with relapsed or refractory AML. Fast unrelated donor search and work up, with conditioning in aplasia allowed a high rate of successful HSCTs. The leukemia-free survival for this group of elderly, high risk AML patients is very promising.
Middeke:Genzyme: Speakers Bureau. Off Label Use: Clofarabine for AML. Schetelig:Genzyme: Research Funding; DKMS German Bone Marrow Donor Center: Employment.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal