Abstract
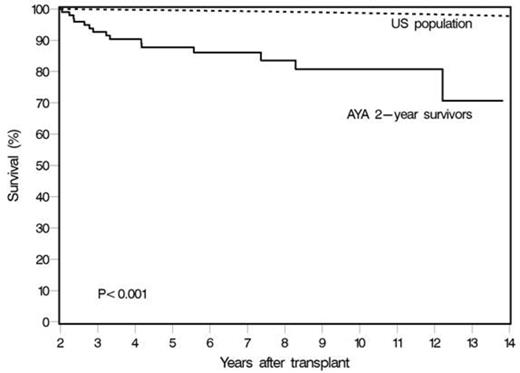
AYAs with cancer have been designated as a vulnerable population by the National Cancer Institute. This group, defined by the ages of 16-39 years, has not enjoyed the same survival improvements over the past several decades as older and younger cohorts. The reasons for outcome disparities among AYA leukemia patients are not well understood. Recent studies have compared outcomes of AYA HCT recipients with younger and older cohorts and reported no lag in survival improvements over time. However, long-term survival after allogeneic HCT in this age group has not been well described. We analyzed outcomes for 226 AYA patients with acute and chronic leukemia, myelodysplastic syndromes, aplastic anemia and lymphoma who were transplanted at our institution from 1/2000-3/2013. The median age at HCT was 29 years (range 15-39) and their median follow up was 5 years (range, <1– 14). Most patients had acute leukemia (65%) and received HCT using related donors (40%) or unrelated donors (60%, including 20 UCB). 92% patients received myeloablative conditioning, most commonly using Bu+Cy±VP16 (50%), TBI+VP16 (17%) or Cy+TBI (13%). Table shows 10 year outcomes in our cohort. The 100 day cumulative incidence of grade 2-4 acute GVHD was 42% (95% CI, 36-49) and 2 year incidence of chronic GVHD was 41% (95% CI, 34-47%). The most common causes of death were relapse (36%), infection (18%) and acute GVHD (14%). In multivariate analyses, risk factors associated with inferior overall survival included greater number of prior chemotherapy regimens, high HCT-CI risk score, presence of active disease at HCT, diagnosis of ALL, MDS or Hodgkin lymphoma, CMV positive serostatus and use of myeloablative conditioning. Since survival started to plateau at 2 years post-transplant, we compared the overall survival of 2 year survivors with that of the general age-, sex- and race-matched general population. Survival continued to remain significantly lower than the general population till 10 years post-HCT (Figure). In conclusion, AYAs who receive allogeneic HCT have favorable long-term survival. However, non-relapse mortality continues to be a significant issue in this population and providers should pay attention to screening and prevention of late complications.
10 year outcomes after allogeneic HCT in AYAs
| . | Probability (95% CI) . |
|---|---|
| Overall survival | 43% (35-50) |
| Relapse free survival | 36% (29-43) |
| Relapse* | 29% (22-35) |
| Non-relapse mortality* | 37% (30-44) |
| Second cancers* | 7% (2-12) |
| . | Probability (95% CI) . |
|---|---|
| Overall survival | 43% (35-50) |
| Relapse free survival | 36% (29-43) |
| Relapse* | 29% (22-35) |
| Non-relapse mortality* | 37% (30-44) |
| Second cancers* | 7% (2-12) |
* Cumulative incidence estimates
Survival of AYA HCT recipients who were alive at 2 years vs. survival of age-, sex-, and race-matched general population
Survival of AYA HCT recipients who were alive at 2 years vs. survival of age-, sex-, and race-matched general population
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal