Abstract
Previous studies have suggested that IKZF1 gene deletions are associated with an adverse prognosis in acute lymphoblastic leukemia (ALL). However, the prognostic value of IKZF1 deletions in adult common B-cell ALL (Com-B ALL) has not been well-defined, especially in the context of different post-remission therapies. The objectives of this study were to evaluate the prognostic role of IKZF1 deletions in adult Com-B ALL.
Overall, 162 untreated adult Com-B ALL patients were recruited between April 2006 and April 2013. Patients received one or two cycles of induction therapy and, if in remission, were allowed to select either ongoing systemic chemotherapy or hematopoietic stem cell transplantation (HSCT). BCR-ABL positive patients were additionally treated with tyrosine kinase inhibitors (TKIs). Deletions in the IKZF1 gene were detected using multiplex RQ-PCR, multiplex fluorescent PCR, multiplex ligation-dependent probe amplification (MLPA) and sequence analysis. High-risk (HR) was defined as having any of the following factors: central nervous system involvement at diagnosis; age ¡Ý50 years; WBC count ¡Ý30x109/L; hypodiploidy; mixed lineage leukemia (MLL) gene rearrangements; BCR-ABL rearrangements; t(1;19) translocations; or a complicated karyotype (¡Ý5 chromosomal abnormalities); failure to achieve remission after two cycles of induction therapy. The study end points included relapse-free survival (RFS), disease-free survival (DFS) and overall survival (OS), which was analyzed using the Kaplan-Meier method. The cumulative incidence of relapse (CIR) was estimated, adjusting for competing risks of death, and compared by Gray's test.
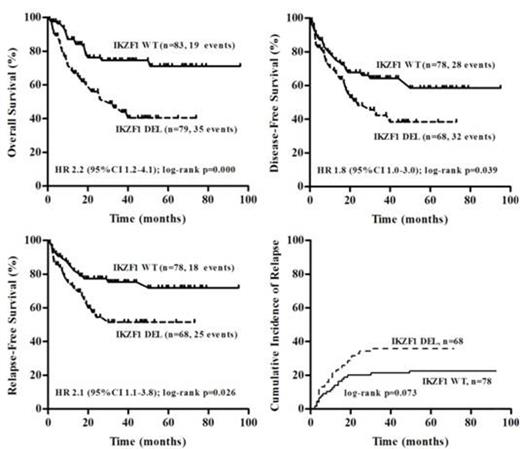
IKZF1 deletions were detected in 79 (48.8%) out of 162 adult Com-B ALL patients. Patients with an IKZF1 deletion (n=79) had a significantly inferior prognosis than those with wild-type IKZF1 (n=83) (Fig.1). The prognosis of patients with IKZF1 deletions with or without the BCR-ABL rearrangements was significantly inferior compared to those of patients with neither IKZF1 deletions nor BCR-ABL rearrangements. The power of IKZF1 deletion status as a prognostic factor remained in both non-HR group (5-yr OS: 52.5%¡À13.1% for IKZF1 deletions (n=25) vs. 72.2%¡À8.8% for wild-type IKZF1 (n=42), P=0.048) and HR group (5-yr OS: 36.7%¡À8.2% for IKZF1 deletions (n=54) vs. 69.3%¡À8.3% for wild-type IKZF1 (n=41), P=0.015). Among patients who received chemotherapy as post-remission therapy (n=52), IKZF1 deletions were associated with an unfavorable OS (P=0.003). In this group, the median OS time for IKZF1-deletion patients (n=28) was 10.0¡À1.0 months, while the median OS time for IKZF1-wild-type carriers (n=24) was not achieved. Among those that received HSCT as post-remission therapy (n=94), IKZF1 status did not affect the prognosis.
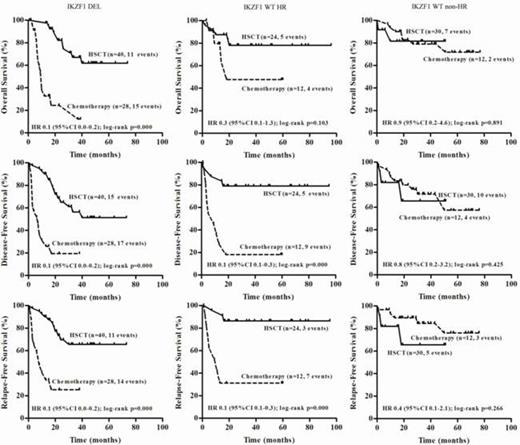
For patients with IKZF1 deletions, HSCT (n=40) was significantly superior to chemotherapy (n=28) as a post-remission therapy. In the wild-type IKZF1 HR group, patients that received HSCT (n=24) achieved a longer DFS and RFS while the OS did not significantly differ from that of patients who received chemotherapy alone (n=12). In the wild-type IKZF1 non-HR group, there was no significant difference between patients that received HSCT (n=30) and those who received chemotherapy (n=12) as a post-remission therapy. Comparing survival curves of HSCT to chemotherapy are shown in Fig.2. Multivariate analysis confirmed the negative impact of IKZF1 deletions on OS (RR 2.3; 95% CI, 1.3-4.3; P=0.007), DFS (RR 1.8; 95% CI, 1.1-3.0; P=0.029), RFS (RR 2.1; 95% CI, 1.3-3.9; P=0.018) and favorable impact of HSCT on OS (RR 0.2; 95% CI, 1.0-0.5; P=0.000), DFS (RR 0.2; 95% CI, 0.1-0.4; P=0.000), RFS (RR 0.2; 95% CI, 0.1-0.4; P=0.000).
These results indicated that IKZF1 status served as an independent negative prognostic marker in adult Com-B ALL and surpassed conventional HR features in the era of TKIs. Patients may benefit from therapy stratified by IKZF1 deletions and conventional HR features.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal