Abstract
Background: Based on cytogenetic and molecular phenotypes, the European LeukemiaNet (ELN) classification is widely accepted for risk stratification of patients with acute myeloid leukemia (AML). Single leukemic blast cell antigens were also shown to have prognostic value, but the influence of AML blast maturity within the different ELN risk groups is largely unknown.
Methods: Our study includes 300 AML patients, who were diagnosed at our institution between 01/2003 and 04/2012 and in whom morphologic, immunophenotypic, cytogenetic and molecular data from primary diagnosis were available. A flow cytometric maturity score was developed in order to distinguish mature AML (AML-ma) from immature AML (AML-im) by means of a quantitative analysis of the expression of early progenitor cell antigens (CD34, CD117, and TdT). Clinical outcome analysis was performed both in the whole cohort and in the different ELN risk groups using Chi Square and Fisher's Exact Test (CR/CRi) and Logrank Test (RFS, OS).
Results: A mature AML blast phenotype (AML-ma) was associated with a significantly longer RFS (7.5 vs. 4.3 years) and OS (5.3 vs. 2.7 years) than an immature phenotype (AML-im) (p < 0.001). Low-risk phenotypes according to ELN (NPM1, PML-RARA) significantly accumulated in the AML-ma group, whereas high-risk aberrations (monosomal and complex aberrant karyotypes, -5 or del(5q), -7) had a higher frequency in AML-im.
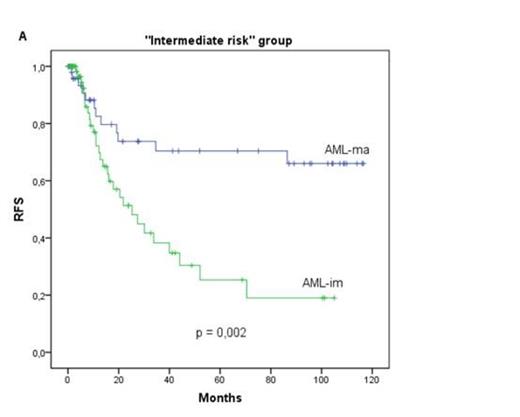
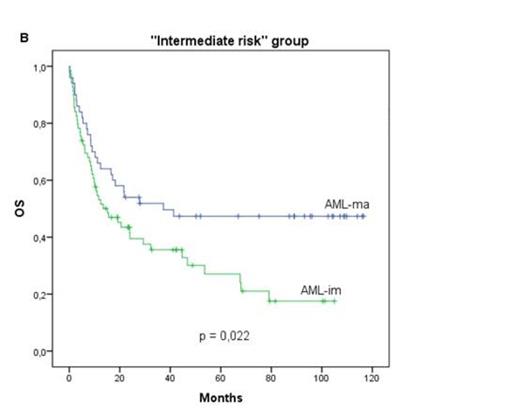
Interestingly, the differences in RFS and OS were maintained in a subgroup analysis within the different ELN risk groups. Statistical significance was obtained in the intermediate risk group with AML-ma being superior to AML-im (RFS: 7.0 years (AML-ma) vs. 3.3 years (AML-im); p = 0.002; OS: 5.1 years (AML-ma) vs. 3.0 years (AML-im); p = 0.022). In contrast, there was no correlation between AML blast maturity and CR/CRi rates.
Conclusions: Our novel flow cytometric score easily determines AML blast maturity and can predict clinical outcome, even within the different ELN risk groups. Particularly for intermediate risk patients according to ELN, the score may be useful in post remission therapy decision-making. It remains to be clarified whether these results reflect differences in genetic instability and/or a different frequency of leukemia stem cells in AML-ma and AML-im.
RFS (A) and OS (B) of AML patients with mature (AML-ma) and immature (AML-im) blast phenotype within the ELN intermediate risk group. AML-ma show a significantly longer RFS and OS compared to AML-im.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal