Abstract

The WHO recognizes a category of B-cell lymphoma, unclassifiable, with features intermediate between DLBCL and cHL, which is commonly referred to as GZL. This is an uncommon entity that is reported to present primarily with mediastinal involvement; there is a paucity of data describing non-mediastinal presentations. Furthermore, treatment of this entity is challenging due to disease heterogeneity, lack of data regarding prognostication, and no standard guidelines for management.
We performed a multicenter retrospective analysis of newly diagnosed GZL patients (pts) treated from 2001-2012 at 18 North American academic centers. Inclusion criteria included availability of clinical information as well as minimum follow up of 12 months for non-relapsing pts. Diagnosis was established by institutional expert pathology review. We examined detailed pt characteristics, treatment and outcome, and we determined prognostic factors associated with survival on univariate and multivariate Cox regression analyses.
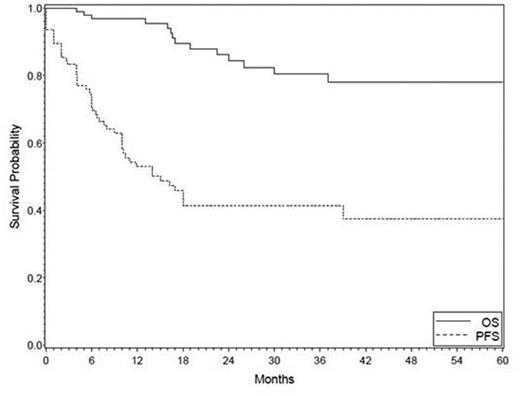
100 pts with GZL were identified; 4 were excluded for inadequate follow-up. Of 96 cases, median age was 39 years (19-86) with 23% of pts age ≥ 60 years; M:F ratio was 1.5:1. Clinical characteristics at diagnosis were as follows: 52% stage III/IV; 56% B symptoms; 89% ECOG PS 0-1; 38% elevated LDH; 31% hypoalbuminemia, 62% anemia; 13% bone marrow involvement; 24% bulky disease >10cm (26% stage I/II and 20% stage III/IV had bulk disease); and 23% of pts had IPI 3-5 and 18% IPS 4-7. Notably, 44% of pts presented with mediastinal involvement (MGZL), while 56% had systemic disease without mediastinal involvement (NMGZL). Compared with NMGZL, pts with MGZL were younger (37 vs 50 years, P<0.0001) and more frequently had stage I/II disease (77% vs 17%, P=0.0001). Further, MGZL had lower IPS (12% 3-7) and IPI scores (12% 3-5) compared with NMGZL (44% IPS 3-7, P=0.0002; and 33% IPI 3-5, P=0.0006). The most common first-line therapy for all pts was R-CHOP (n=48), followed by ABVD (n=25), R-EPOCH (n=10), CHOP (n=5), BEACOPP or hyperCVAD (n=5), and other (n=2); 69% of pts received rituximab as part of first-line therapy and 31% received consolidative radiotherapy (RT) (RT: 70% of MGZL and 13% of NMGZL). The overall response rate (ORR) to first-line therapy was 70% with 58% achieving a complete remission (CR); 27% of pts had primary refractory disease. While there was a trend for improved CR rate for pts who received rituximab as part of first-line therapy (65% vs 40% for those not receiving rituximab, P=0.07), there were no significant differences in response based on other individual treatment regimens or modalities. At a median follow-up of 25 months (8-109), the 2-year progression-free survival (PFS) and overall survival (OS) for all pts were 41% and 84%, respectively (Figure 1). PFS and OS were superior for pts with stage I/II disease compared with stage III/IV (PFS: 52% vs 32%, respectively, P=0.02; OS: 97% and 71%, respectively, P=0.001). On univariate analysis, clinical factors that predicted PFS and OS are detailed in Table 1. Interestingly, despite having lower risk features, the PFS or OS for MGZL did not differ from NMGZL. On multivariate regression analysis for PFS, elevated LDH was the only factor that predicted poorer outcome (HR 2.01 (95% CI 0.99-4.09), P=0.05). Several factors were significant for inferior OS including: presence of B symptoms (HR 17.41 (95% CI 1.53-197.57), P=0.02), hypoalbuminemia (HR 8.09 (95% CI 1.37-47.83), P=0.02), and stage 4 vs 1-3 disease (HR 21.39 (95% CI 2.90-157.74), P=0.003).
Survival of Newly-Diagnosed GZL (n=96).
To the best of our knowledge, this is the largest series of GZL reported to date. We describe a new clinical subtype (NMGZL), which has distinct characteristics, but similar outcomes as MGZL. Within the limitations of a retrospective analysis, overall PFS appeared inferior to that observed in cHL and DLBCL, though OS was excellent, suggesting in part the success of salvage therapy. An elevated LDH was associated with worse PFS, while there were no differences seen based on clinical presentation or initial therapy. Further, there were several clinical factors identified (i.e., B symptoms, albumin, and stage) that strongly predicted OS. Continued examination both biologically and clinically of this unique subset of lymphoma is warranted.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This icon denotes a clinically relevant abstract


This feature is available to Subscribers Only
Sign In or Create an Account Close Modal