Abstract
many aspects should be considered when selecting an ideal donor. The progress made in haploidentical HSCT in recent years offers almost unlimited donor and availabilities of more than one donor at many occasions. To date, there have been no studies to answer the question of apart from HLA disparity, whether one donor should be preferred over another among various haploidentical donors available. The goal of the current study was to attempt to answer the question by analyzing the data on haploidentical HSCT without in-vitro T cell depletion modality.
Consecutive patients with leukemia or MDS who received HSCT from 3-5 of 6 HLA loci-matched family donors excluding collateral relatives between May 2002 and December 2010 were enrolled in this study (n=749). The stem cell source was G-CSF mobilized BM combined with PB. The conditioning regimen was modified BUCY plus ATG with 10mg/kg in total dosage. Patients receiving prophylactic DLI for prevention of leukemia relapse were excluded. Donor-recipient risk factors relevant to selection of optimal donor for haploidentical HCT were analyzed.
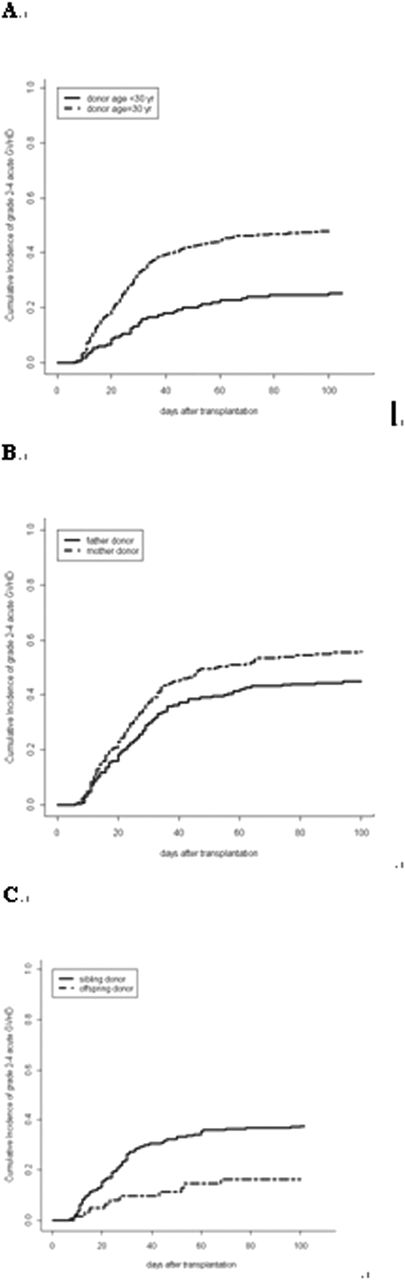
(1)donor sex: male donor had lower incidence of both grade 2-4 (39% vs. 46%, p=.07) and grade 3-4 acute GVHD (aGVHD) (11% vs. 17%, p=.04), lower rate of NRM (16% vs. 24%, p=.006) and higher probabilities of OS (70% vs. 62%, p=.02) and LFS (67% vs. 60%, p=.03), compared with female donor. In multivariate analysis, donor sex was still a risk factor for GVHD, NRM and survival. However, if mother donor was excluded, all the difference became no longer significant. (2) Donor age: donor younger than 30 years old had lower incidence of both grade 2-4 (25% vs. 48%, p<.0001) and grade 3-4 aGVHD (5% vs. 16%, p=.0005), lower rate of NRM (12% vs. 22%, p=.007) and higher probabilities of OS (78% vs. 64%, p=.001) and LFS (76% vs. 64%, p=.002), compared with donor older than 30 years old. In multivariate analysis, donor age was a more prominent risk factor for GVHD, NRM and survival compared with donor sex. And if mother donor was excluded, all the difference remained significant both in univariate and multivariate analysis. (3)The rate of GVHD was not associated with the extent of HLA disparity or any individual allele disparity. (4) comparison between mother and father: father donor had lower incidence of both grade 2-4 (45% vs. 56%, p=.03) and grade 3-4 aGVHD (13% vs. 22%, p=.007), lower rate of NRM (14% vs. 26%, p=.003) and higher probabilities of OS (70% vs. 57%, p=.007) and LFS (67% vs. 57%, p=.03), compared with mother donor. In multivariate analysis, mother donor was still a risk factor for GVHD, NRM and survival. (5) comparison between offspring and sibling: offspring donor had significant lower incidence of grade 2-4 aGVHD (16% vs. 37%, p=.002), lower NRM and higher survival, although not reaching statistical significance, compared with sibling donor. In multivariate analysis, sibling donor was still a risk factor for GVHD. (6) comparison among sibling and father donors: donor older than 30 years old was the most important risk factor affecting GVHD, NRM and survival while the rates between father and sibling donor were comparable.
Not abiding by the rule of HLA disparity, this study was the first one to confirm that significant different outcomes were achieved among various haploidentical donors and proved once again that haploidentical HSCT overcame HLA barriers. Instead of HLA disparity, donor age and the family relationship were important risk factors under our treatment modality. The underlying mechanisms of crossing human leukocyte antigen barriers need further investigation and to be validated by other treatment modalities.
Figure impact of donor age and family relationship on GVHD
This work was partly supported by The Key Program of National Natural Science Foundation of China (Grant No. 81230013), Beijing Municipal Science & Technology Commission (No.Z121107002812033) and Beijing Municipal Science & Technology Commission(No. Z121107002612035).
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal