Abstract
Granulocyte-colony stimulating factor (G-CSF) is the prototypic agent used to mobilize hematopoietic stem and progenitor cells (HSPCs) into the blood where they can then be harvested for stem cell transplantation. G-CSF acts in a non-cell-intrinsic fashion to induce HSPC mobilization. We recently showed that G-CSF signaling in a CD68+ monocyte/macrophage lineage cell within the bone marrow initiates the HSPC mobilization cascade (Christopher et al., 2011). CD68 marks a heterogeneous cell population that includes monocytes, macrophages, myeloid dendritic cells, and osteoclasts. Within the bone marrow, myeloid dendritic cells (MDCs) are found perivascularly and in close association with CXCL12-abundant reticular (CAR) cells, suggesting a role for MDCs in maintaining HSPC niche function. We previously reported that G-CSF treatment (250 µg/kg per day for 5 days) suppresses macrophage (11.8 ± 3.6-fold) and myeloid dendritic cell (MDCs; 5.5 ± 1.2-fold) numbers in the bone marrow (Supakorndej et al., ASH abstract #2319, 2012). Moreover, we showed that CD11c-DTR mediated MDC ablation results in a modest mobilization of HSPCs. However, CD11c-DTR ablates bone marrow macrophages, as well as MDCs, so a definitive role for MDCs in G-CSF-induced HSPC mobilization could not be established.
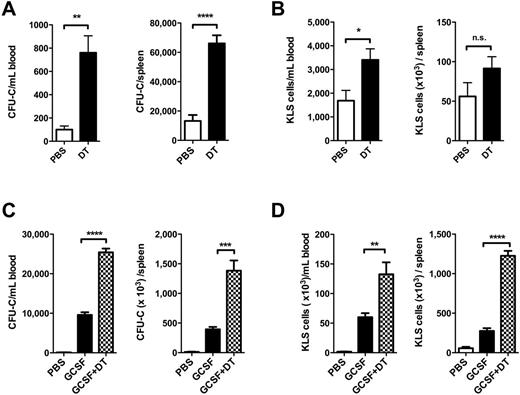
HSPC mobilization in Zbtb46-DTR mice. Zbtb46-DTR bone marrow chimeras were treated with diphtheria toxin (DT) alone, G-CSF alone, or DT plus G-CSF. The number of CFU-C (A & C) or KLS cells (B & D) in the blood and spleen are shown. Data represent the mean ± SEM of 5 mice from one experiment. *p < 0.05; **p < 0.01; ***p < 0.001; ****p < 0.0001.
HSPC mobilization in Zbtb46-DTR mice. Zbtb46-DTR bone marrow chimeras were treated with diphtheria toxin (DT) alone, G-CSF alone, or DT plus G-CSF. The number of CFU-C (A & C) or KLS cells (B & D) in the blood and spleen are shown. Data represent the mean ± SEM of 5 mice from one experiment. *p < 0.05; **p < 0.01; ***p < 0.001; ****p < 0.0001.
We previously showed that G-CSF mobilizes HSPCs, at least in part, by decreasing CXCL12 expression in bone marrow stromal cells. We found that MDC ablation (using CD11c-DTR mice) also suppresses CXCL12 expression in the bone marrow (35.2 ± 18.1% reduction). We recently reported that CXCL12 expression from perivascular stromal cells (including mesenchymal progenitors, CAR cells, and endothelial cells) is required for HSC maintenance (Greenbaum et al., 2013). Here, we show that G-CSF suppresses CXCL12 mRNA expression in both CAR cells and endothelial cells. Surprisingly, preliminary data suggest that MDC ablation does not affect CAR cell number nor CXCL12 expression in these cells. Studies are in progress to assess the effect of MDC ablation on endothelial CXCL12 expression. Collectively, these data suggest that MDC-derived signals contribute to HSPC maintenance by modulating stromal cells that comprise the perivascular niche.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal