Abstract
Despite the great clinical benefit from the advent of tyrosine-kinase inhibitors (TKIs) treatment for adult patients with Philadelphia-positive acute lymphoblastic leukemia (Ph+ ALL), allogeneic hematopoietic stem cells transplantation (allo-HSCT) does not appear to be dispensable, if the optimal long-term outcome is to be achieved. However, there are only few data reported on long-term survivors with Ph+ ALL, particularly for those not receiving pre-transplant TKIs in the conventional induction therapy.
In this retrospective analysis, we report on the long term outcomes of myeloablative allo-HSCT during the past 2 decades as single center experience. Data on the use of post-transplant TKIs and molecular monitoring for minimal residual disease are being collected to investigate their predictive role.
Between 1989 and 2013, we collected 56 patients who underwent myeloablative allo-HSCT from HLA-identical siblings (n: 24), unrelated donors (n: 17), alternative donors (n: 15). Median age was 41 years (16-64). Disease phase at transplant was CR1 in 30 pts (53%), >CR1 in 26 pts. Pre-transplant TKI as part of induction therapy was given in 25 pts (44%). Conditioning regimen was TBI-based in 47 pts (83%) and chemotherapy-based in 9 pts. GVHD prophylaxis was given according to Center standard practice.
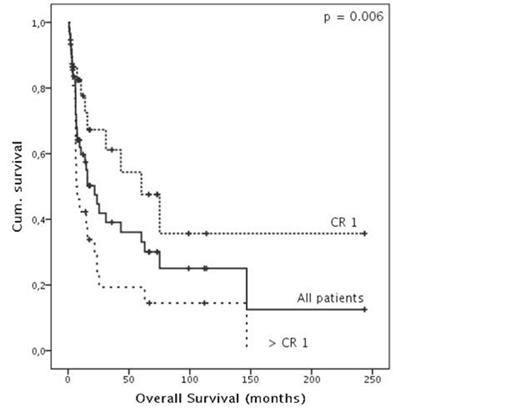
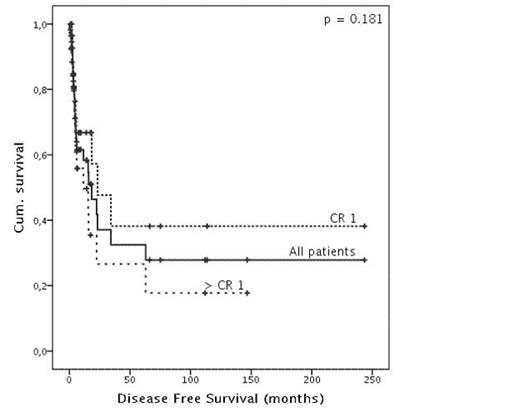
Median follow-up was 67 months (1- 244). There were no cases of primary graft failure. Incidence of grade II-IV acute GVHD occurred in 31 pts (55%) and extensive chronic GVHD in 18 pts (32%). Transplant-related mortality was 35% at 2 years and 7 more patients died of non-relapse causes up to 12 years after transplant. The 10-year OS was 25% and significantly better for patients in CR1 vs. >CR1 (36% VS 14% - p=0,006). The 10-year DFS was 27% with no statistical difference for pts in CR1 vs. >CR1. Age at transplant and pre-transplant TKI did not affect the outcomes.
In this retrospective analysis over a 20-year time period, we show that approximately one-third of adult Ph+ ALL are cured if they undergo allo-HSCT in CR1. Therefore, we confirm that disease status at transplant has a major prognostic impact on clinical outcomes. The apparent lack of benefit of pre-transplant TKI exposure may be due to the retrospective nature of the analysis.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal