Abstract
Allogeneic hematopoietic stem cell transplantation (HDT) in the elderly patient with acute myeloid leukemia (AML) or myelodysplasia (MDS) continues to pose a challenge due to treatment failure and treatment related toxicity. TBI/Cy, allows for engraftment and tolerance while maximizing anti-tumor activity, but can be a difficult regimen in elderly patients due to its associated toxicity profile. The introduction of reduced intensity conditioning regimens (RIC) and improved supportive care has led to decreased mortality following HDT in the elderly. However, for patients at high risk for relapse, RIC may not achieve prolonged disease control. For these patients, an ablative HDT with reduced toxicity (RT-SCT) may be beneficial by controlling disease with acceptable toxicity while allowing a GVL effect. We evaluated a novel conditioning regimen in an open label phase II study consisting of Bu/Pent aimed at improving toxicity, relapse rate, and overall survival (OS) in elderly patients with AML or MDS, and compared them with an elderly group who received TBI/Cy.
We treated 54 patients with AML/MDS over the age of 55, who were recipients of HDT from fully matched related donor (MRD), umbilical cord donor, or matched unrelated donor (MUD). We defined elderly as greater than 55 years of age. The median age in the Bu/Pent group was 64, 61% had adverse prognostic features including cytogenetics, relapsed, treatment related or transformed disease, or high IPSS score, 39% were in the intermediate group. There were 60% MRD and 40% unrelated HDT. In the TBI group median age was 59, 48% had adverse features and 52% intermediate, 48% MRD and 52% unrelated HDT.
The Bu/Pent group (n=23) was conditioned with intravenous busulfan 1.6mg/kg every 12 hours day -7 to -4 and pentostatin 4mg/m2 on day -3 and day-2 prior to SCT on day 0. GVHD prophylaxis was methotrexate 10mg/m2 on day 1 and 5mg/m2 on days 3 and 6. Tacrolimus was started on day -2 and tapered over 1 month after day +100. Relapse, survival and toxicity data was compared with a historical control group at our institution who received 12 Gy TBI/Cy (60 mg/kg x 2) (n=31). Controls were selected by retrospective chart review of patients with a diagnosis of MDS or AML who had received an allogeneic transplant with a TBI/Cy based conditioning regimen after the age of 55.
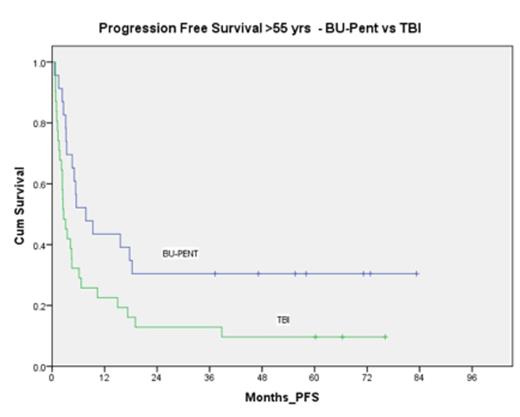
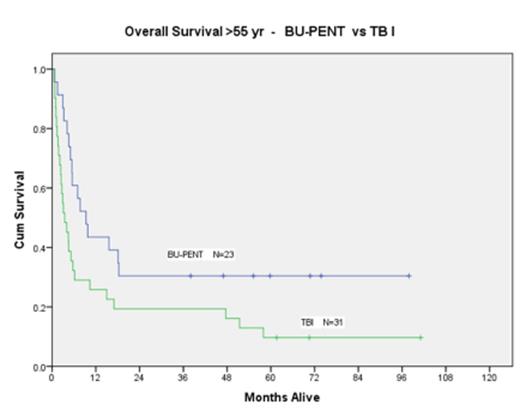
There was no graft failure reported in either group. The OS at 100 days and 1-year post HDT was significantly better for the Bu/Pent group vs. TBI group (82.6% vs. 51.6% and 43.5% vs. 25.8% respectively; p value= 0.029). Progression free survival (PFS) was also significantly better in the elderly population receiving Bu/Pent; 43.5% at 1 year versus 22.6% in the TBI group with a p value of .021. The rate of relapse was comparable regardless of conditioning regimen with 34% in the Bu/Pent group (8/23) and 29% in the TBI/Cy group (9/31) relapsing.
Transplant related mortality (TRM) accounted for 13% (3/23) of the deaths in the Bu/Pent group, and 38% (12/31) in the TBI/Cy group. Of the three deaths in the Bu/Pent group, 2 were due to GVHD and 1 was secondary to sepsis within 100 days. Other significant nonfatal toxicities such as mucositis and nausea/vomiting were medically managed and rates of GVHD were similar in the two groups; 10/23 (43%) in the Bu/Pent group and 14/31 (45%) in the TBI group. Of the 10 GVHD patients in the Bu/Pent group, 7 had chronic (cGVHD) (30%). None of the patients in the Bu/Pent group and 3/31 in the TBI group developed VOD.
Upon sub-group analysis, elderly CIBMTR high-risk AML/MDS patients who received Bu/Pent had an 86% 100 day survival versus 60% in the TBI/Cy group; 1 year survival was 43% and 33% respectively. In the elderly CIBMTR intermediate risk group, Bu/Pent 100 day survival was 78% vs. 44% in the TBI group. At 1 year, patients in the intermediate group who received Bu/Pent had 45% survival vs. 19% in the TBI group.
We found that OS and PFS at 100 days and 1 year were significantly better in the Bu/Pent group due to a much lower TRM. The Bu/Pent based regimen appears to be superior for patients over the age of 55 with MDS or AML undergoing HDT when compared with TBI based regimens. With a low toxicity profile, Bu/Pent patients had a lower incidence of TRM when compared with a prospective study of patients receiving RIC-SCT busulfan/fludarabine (20%) and a lower incidence of cGVHD(53%) (Valcarcel et al). This regimen warrants further prospective evaluation.
p value= 0.029
p value= 0.021
Smith:Seattle Genetics, Inc.: Research Funding; Spectrum: Consultancy; Cephalon: Consultancy, Speakers Bureau; Celgene: Consultancy, Speakers Bureau; GlaxoSmith Kline: Speakers Bureau. Rodriguez:otsuka: Honoraria, Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal