Abstract
Conservative treatment which typically includes phlebotomy or hydroxyurea or other cytoreductive therapy (plus aspirin) (ConsRxAsa) is effective treatment with acceptable complications for management of polycythemia Vera (PV) but is not considered curative [thus resulting in a shorter life expectancy (LE) in comparison to LE in the general population]. On the other hand, an allogeneic hematopoietic cell transplantation (allo-HCT) from a HLA compatible donor is considered a curative treatment option, but is potentially associated with high-risk of life-threatening complications. We sought to answer the question of which of these two treatment options results in better survival.
Because there are no direct randomized controlled trials (RCT) addressing the question if ConsRxAsa is superior to allo-HCT, we resorted to a decision-analysis to answer this question. We constructed a Markov model to represent and analyze the decision of ConsRxAsa vs. Allo-HCT. The results of the model were expressed in terms of life expectancy (LE) and survival probabilities. We performed a systematic review (and when possible a meta-analysis) to inform parameters in the model. ConsRxAsa arm was modeled by simulating the natural history of PV. For Allo-HCT arm, we adopted our previously published model (Biol Blood Marrow Transplant 2009;15:1415-21) but modified it to evaluate the effect of both conventional and reduced-intensity allo-HCT performed in chronic phase of PV.
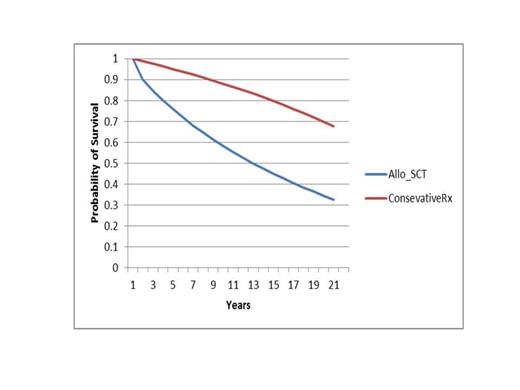
We identified 165 relevant articles of which only 7 described testing various treatments for PV in RCTs. However, most data used to populate the decision model came from one RCT and one cohort study. Using base case of age of 45 years, we estimated a probability of survival at 10 and 20 years of 86% and 67% for ConsRxAsa versus 55% and 32% for allo-HCT (Fig). This translates into an average LE of 17.1 years for ConsRxAsa vs. 11.6 years for allo-HCT, respectively. Sensitivity analysis according to age, early transplant-related mortality, risk of bleeding or thrombosis did not affect the results. Adopting median age of 65 years and comparing reduced-intensity allo-HCT vs. ConsRxAsa, we found that the average LE was 8.6 years for allo-HCT vs. 12.5 in the conservative treatment arm. Again, conservative treatment remained superior under a wide range of assumptions.
integration of current best existing evidence into the decision model shows that conservative management of PV appears to provide a better survival compared to offering an allo-HCT in chronic phase of P. Vera.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal