Abstract
Since the IRIS Study in 2000, tyrosine kinase inhibitors (TKI) have become a standard therapy for CML patients in lieu of interferon based therapy. Nevertheless, resistance occurs in roughly 30% of imatinib-treated patients. This resistance is attributable to ABL kinase domain mutations in 50% of cases, in which T315I mutation accounts for 10 to 15%. This latter is resistant to all TKIs available except for ponatinib which enables 75% of complete cytogenetic response (CCyR) in this setting (NEJM November 29, 2012). Before Ponatinib, various strategies were proposed to overcome the T315I mutation including more importantly ‘non-targeted' therapy such as Omacetaxine. IFN is also a ‘non-targeted therapy' known to have a well-established immunological effect. There are also clues about its cellular effects: microarray analyses have shown that IFN alfa can upregulate genes that encode for apoptotic proteins (i.e TRAIL, Fas, caspases 4 and 8 and XAF-1…) conferring the anti-growth effect different from ATP competition specific to TKIs.
We report here an 80 years-old imatinib-resistant CML patient harboring the T315I mutation who has been successfully treated with Peg-IFN (Pegasys).
His past medical history involved hypertension, asthma and chronic obstructive pulmonary disease. He was diagnosed in July 2008 with a chronic phase CML when he presented with weight loss, splenomegaly, leukocytosis (WBC 80G/l), slight anemia (Hemoglobin 112G/l) and normal Platelet count 240G/L. Karyotyping of 26 metaphase cells in the bone marrow showed Philadelphia (Ph1) chromosome without any additional abnormality. The molecular analysis by real time PCR (Light Cycler 480) detected a BCR-ABL p210 transcript. The Sokal score was high (at 1.24) while the Eutos score was low (31).
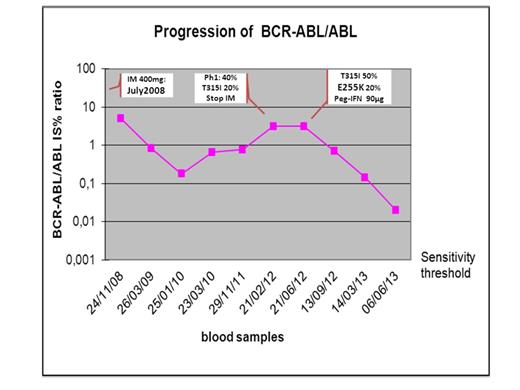
He started Imatinib 400mg daily in July 2008 and achieved 5% IS BCR-ABL ratio at 3 months and complete cytogenetic response (CCyR) at 12 months. But the patient had never reached the major molecular response (MMR) and ended up losing the cytogenetic response in February 2012 (at 40 months) with an increase of 1.5log in the BCR-ABL ratio. Sequencing analysis for ABL mutation was carried out using the applied biosystems 3500 gentic analyzer. It revealed the T315I mutation at 20%. After a request for Ponatinib was dismissed by our health authorities, we decided to treat the patient with Peg-IFN in June 2012 at the dose of 90 µg per week. At this point, the imatinib had been stopped for 3 months, 8 metaphase cells out of 20 showed Ph1 chromosome without additional abnormality, BCR-ABL ratio was 3% IS, the mutational analysis showed 50% of T315I and 20% of another acquired E255K mutation. But the patient was still in complete haematologic response. figure 1 highlights the decline in the BCR-ABL ratio with MMR reached for the first time at 9 months (from Peg-IFN treatment). Of note, the CCyR was obtained again at this landmark. At 12 months from the Peg-IFN the CCyR was confirmed, the BCR-ABL ratio came very close to MMR4 (0.02% IS) while both T315I and E255K mutations disappeared on mutational analysis.
No side effect was reported except for weight loss when the dose of Peg-IFN was increased to 180 µg per week which was the dose suggested by J.H. Lipton (Leukemia and Lymphoma, March 2007). The average dose in the past 12 months was 90 µg per week. The latter dose is well tolerated and is still ongoing.
This observation shows that, though we are in the ponatinib era, there still is a room for interferon, in the management of CP CML patients even in BCR-ABL domain mutated patients because of its different mechanism of action. In this case the Pegylated Interferon a-2-a at the dose of 90µg per week has allowed clearance of both T315I and E255K mutations with a response close to MMR4. Taking into account the slope of the BCR-ABL decline, deeper molecular response is expected before the ASH meeting in December 2013.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal