Abstract
AL amyloidosis, precipitated by the deposition of immunoglobulin light chains in various organs, is generally secondary to the benign or malignant proliferation of clonal plasma cells. Reviews from large amyloid centers show that approximately 2-3% of AL amyloidosis is associated with an underlying non-Hodgkin lymphoma (NHL). Of the non-Hodgkin lymphomas, lymphoplasmacytic lymphoma (LPL) is most commonly associated with systemic AL amyloidosis. Systemic NHL-associated AL amyloidosis tends to feature a high level of IgM paraproteinemia and a predilection for several different organ tropisms. Here we report the unique case of a 71-year-old male with an insidious course of hypotension and worsening renal failure of unknown etiology, who was ultimately diagnosed post-mortem with AL amyloidosis associated with an intravascular large B-cell lymphoma (IVLBCL).
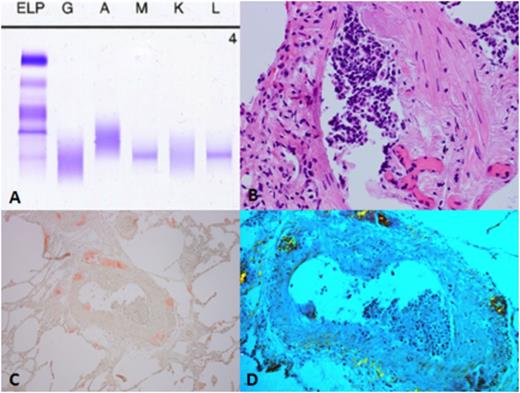
A 71-year-old white male presented to the hospital after a fall. His medical history included type II diabetes, spinal stenosis, and a 30-pack-year smoking history. Over the past few months, he noticed a steady decline in functional status. On admission, he was hypotensive with bilateral 2+ pitting lower extremity edema. Laboratory evaluation revealed leukocytosis, anemia, and acute kidney injury with elevated creatinine and blood urea nitrogen. Urinalysis showed 30 mg/dL of protein, along with the presence of white and red blood cells and moderate bacteria. Enterococcus was subsequently cultured from the urine. A chest X-ray revealed small bilateral effusions. The patient was treated for urosepsis with antibiotics and vasopressor support in the intensive care unit. His hypotension improved initially, but over the next 3 weeks his course was complicated by recurrent episodes of hypotension, altered mental status, and worsening renal function. An exhaustive laboratory workup was negative for infection, and a transthoracic echocardiogram showed no significant findings. Further evaluation included a normal cortisol stimulation test and TSH level, but a serum protein electrophoresis showed 0.13 g/dL of monoclonal IgM lambda immunoglobulin (Figure A) with a urine protein electrophoresis showing a low level of lambda free light chains. Abdominal fat pad biopsy was negative for amyloid. The patient's condition continued to deteriorate, and he died on hospital day 29 with no clear diagnosis. Post-mortem examination revealed a CD20+, lambda restricted intravascular diffuse large B-cell lymphoma involving the kidneys, prostate, a cecal polyp, and lungs (Figure B). Sections of lung tissue revealed scattered areas of extracellular eosinophilic material that stained brick red with Congo red staining (Figure C) and displayed apple green birefringence under polarized light (Figure D). Similar findings in the heart and kidneys were consistent with systemic amyloidosis. Bone marrow analysis showed normal trilineage hematopoiesis with no evidence for involvement by lymphoma or plasma cell neoplasm.
This case exhibits the first reported association of two rare and diagnostically challenging disorders: intravascular large B-cell lymphoma (IVLBCL) and systemic AL amyloidosis. Patients with IVLBCL often present with nonspecific symptoms secondary to small vessel occlusion and subacute deterioration in performance status, as was the case with our patient. Our patient's underlying intravascular NHL with systemic AL amyloidosis proved difficult to diagnose with his low-level IgM paraproteinemia serving as the only clue to the cause of his illness. The negative fat pad biopsy added to the diagnostic difficulty, but was not surprising due to the low sensitivity of the test in detecting systemic amyloidosis. In addition, diagnosing intravascular lymphoma is difficult as patients present with nonspecific findings and often without lymphadenopathy, making post-mortem diagnosis common. Thus, this case sets a precedent for intravascular diffuse large B-cell lymphoma provoking the onset of systemic AL amyloidosis – a covert, morbid, and diagnostically challenging combination.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal