Abstract
Diffuse large B cell lymphoma (DLBCL) is the most common subtype of non-Hodgkin lymphoma (NHL) accounting for approximately 25 percent of NHL cases. It is increasingly appreciated that the diagnostic category of DLBCL is quite heterogeneous in terms of morphology, genetics, and biologic behavior. Patients with DLBCL typically present with a rapidly enlarging lymph node. Extra nodal disease can also occur anywhere in the body and usually denotes an advanced stage.
Approximately 60 percent of patients will present with advanced stage DLBCL (stage III or IV disease). The bone marrow (BM) involvement, as a part of systemic multifocal disease, at presentation is 8-10%, but can be up to 30% during the course of the disease, especially if discordant histologic subtypes, such as follicular lymphoma, are included. BM involvement is a negative prognostic factor of DLBCL despite modern therapy. Primary bone marrow lymphoma (PBML) is a very rare entity in which clinicobiological significance is not well defined, but perceived to represent a particularly poor-risk subclass. Herein, we present a case of primary bone marrow DLBCL and try to explore the unique presentation based on DLBCL-bone marrow microenvironment interactions. Cadherins, for example, are transmembrane proteins that play important roles in cell adhesion and are recently recognized as a component of myeloma and leukemia-bone marrow microenvironment interactions. We hypothesized that DLBCL cells would express N-cadherin. In this study, we evaluated E -cadherin and N-cadherin expression in BM samples from this patient.
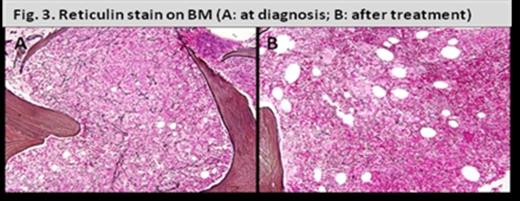
A 77-year-old presented with progressive fatigue, and rapidly developed pancytopenia with transfusion dependence over 3 months. He had no bone pain or B symptoms at presentation. Clinical examination revealed pallor, but no lymph node enlargement or abdominal organomegaly. His hemoglobin was 5.7 g/dL, Platelets 29 X103/µL, and absolute neutrophil count 800/ µL. LDH was elevated at 444 UL. A BM aspirate was a dry tap, BM biopsy showed hyper cellular marrow (90-100%), and greater than 90% involvement by malignant lymphocytes that were positive for CD20, CD79a, Pax5, CD45, NSE, Mum1, and vimentin. Only 5% Mib1 proliferation index was appreciated on the biopsy specimen, probably due to decalcification effect. There was moderately increased reticulin fibrosis. The morphologic and immunophenotypic features were consistent with DLBCL. Cytogenetic studies showed a complex near-triploid abnormal clone. FISH analysis showed no evidence of MYC rearrangement, t(14;18), or t(11;14).
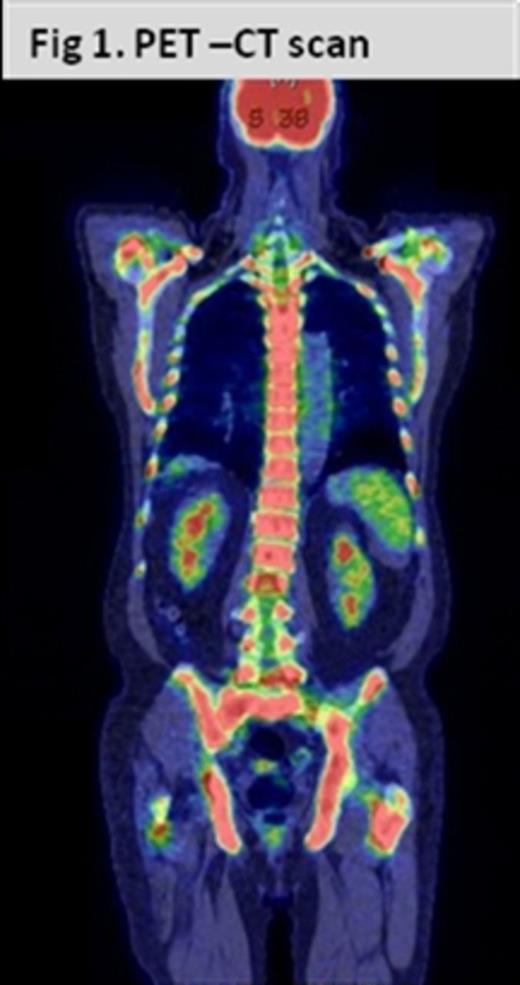
PET-CT scan showed marked increase in metabolic activity diffusely involving the axial skeleton but no metabolically active lymphadenopathy or extramedullary disease, no destructive or lytic lesions were found [Fig.1].
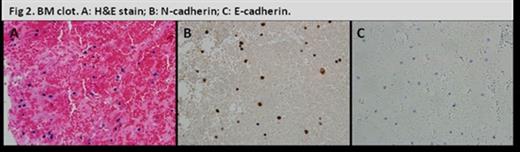
Immunohistochemistry stains showed strong N-cadherin staining the malignant cells [Fig.2]. E-cadherin staining was negative.
The patient was treated with 6 cycles of R-CHOP. Doxorubicin dose was reduced due to advanced age. His post-treatment BM biopsy and PET scan were consistent with complete response. BM fibrosis significantly decreased [Fig. 3]. His cytopenias completely corrected early during therapy.
Criteria to diagnose PBML encompass isolated bone marrow infiltration, with no evidence of nodal or extranodal involvement, including the bone, and the exclusion of leukemia/lymphomas that are considered to primarily involve the bone marrow. In a retrospectively reviewed by the International Extranodal Lymphoma Study Group from 12 institutions in 7 different countries over a 25-year period, there were only 15 cases of DLBCL that met these criteria. The biology behind the exclusive confinement to the BM compartment remains elusive.
On further analysis of this case, E-cadherin was negative. Expression of the adhesion molecule marker N-cadherin on lymphoma cells might help explain the confinement to the BM microenvironment in our case. Future studies should focus on exploring the role of N-cadherin in this rare entity of DLBCL.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal