Abstract
Mantle-cell lymphoma (MCL) is a rare B-cell malignancy that usually presents in stage III-IV disease (classical) with poor outcomes even with aggressive therapy. Rarely, patients present with localized disease and the role of localized or systemic therapy remains a clinical choice.
To assess outcomes in our patients with early stage MCL with a focus on treatment approaches.
Patients with early stage (Ann Arbor Stage I or II) between 1992 and 2012 were identified through our MCL database. Demographic , treatment, and outcomes data was collected for each patient. Cox regression was used to identify risk factors for progression and survival. Kaplan-Meier (KM) method was used to estimate median time to progression (TTP) and overall survival (OS), and comparisons were estimated using the log rank test. A p-value of <0.05 was considered significant.
From our database of 300 patients with MCL, 34 were identified to have stage I or II disease (Table 1). 7 received local therapy, consisting of either radiation or resection. 20 received systemic therapy, including 1 who received only rituximab. 7 received a combination of local therapy and systemic therapy, including 2 who received rituximab with radiation.
Demographic data in patients with early stage MCL
| Characteristics (N=34) | Result | |
| Age in years (median) | 64 (46-84) | |
| WBC in k/uL (median) | 7.6 (4.9-53.2) | |
| % Male | 74% | |
| % Stage I | 56% | |
| % B symptoms | 6% | |
| % Bulky (>5cm) | 12% | |
| % Blastoid/Pleomorophic | 24% | |
| % Extranodal GI NP/OP Testicular Lung/Breast | 62% 38% 38% 14% 10% | |
| ECOG 0-1 | 100% | |
| MIPI Int/High | 42%/16% | |
| Staging | CT PET Marrow Endoscopy | 100% 71% 85% 38% |
| Treatment | Local Systemic Combined | 21% 59% 21% |
| Characteristics (N=34) | Result | |
| Age in years (median) | 64 (46-84) | |
| WBC in k/uL (median) | 7.6 (4.9-53.2) | |
| % Male | 74% | |
| % Stage I | 56% | |
| % B symptoms | 6% | |
| % Bulky (>5cm) | 12% | |
| % Blastoid/Pleomorophic | 24% | |
| % Extranodal GI NP/OP Testicular Lung/Breast | 62% 38% 38% 14% 10% | |
| ECOG 0-1 | 100% | |
| MIPI Int/High | 42%/16% | |
| Staging | CT PET Marrow Endoscopy | 100% 71% 85% 38% |
| Treatment | Local Systemic Combined | 21% 59% 21% |
GI: stomach/intestines; NP: nasopharynx, OP: oropharynx; MIPI: Mantle Cell International Prognostic Index
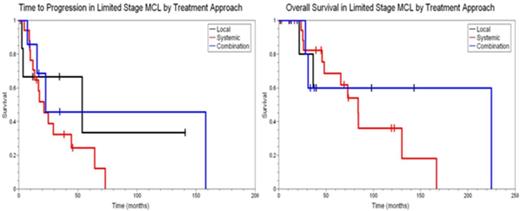
With a median followup of 73.7 months, TTP was 22.8 months and OS was 83.8 months. MIPI could be determined for 56% of the cohort, however, was neither prognostic for TTP or OS. WBC was available for 74% of the cohort, and was prognostic for OS only [HR 1.46 (95%CI 1.02-2.08, p-value=0.04)]. None of the remaining MIPI covariates were prognostic. Ki67 was reported for only 8 patients limiting analysis as a continuous variable. Blastoid/Pleomorphic histology, alternatively, was prognostic for OS [HR 24.5 (95%CI 1.22-25.72, p-value=0.03)], but not TTP. Locally directed therapy was not associated with a decrease in OS or TTP, with some patients showing no evidence of relapse with extended followup (figure 1).
In our series patients with early stage MCL demonstrated a longer TTP and OS than those with extensive stage disease. The MIPI failed to stratify patients, likely related to small sample size. Aggressive histology may confer a worse prognosis, though, it remains unclear whether this can be abrogated by more intensive management, as all with blastoid/pleomorphic histology received some form of systemic therapy. Notably, as described by others, locally directed therapy did not compromise outcomes, with some showing extended TTP and OS.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal