Abstract
Follicular lymphoma (FL) is characterized by clinical heterogeneity. There is a need for easily quantifiable prognostic biomarkers. No consensus has been achieved regarding the prognostic significance of the microvessel density, number of macrophages and cytotoxic lymphocytes within the tumor.
To characterize the microvessel density, number of macrophages and cytotoxic lymphocytes within tumor tissue using immunohistochemical (IHC) analysis of sections from paraffin blocks of lymph node biopsies in two groups of patients with different clinical courses of FL.
The study included 59 patients with FL: 39 women (67%) and 20 men (33%). The median age was 53 years (range: 27–83 years). Forty nine patients were observed in the National Research Center for Hematology (Moscow), and 10 patients in Cancer Research Center (Moscow), from April 2001 until May 2011. Group 1, “good outcome”, included 28 patients who were followed for 2 or more years after the therapy, had remission, or developed relapse in five or more years from the start of treatment (late relapse). Group 2, “poor outcome”, included 31 patients who died due to tumor progression in the first 1–2 years from the time of diagnosis, had primary tumor resistance, or developed FL relapse in the first year from the start of treatment (early relapse). Patients in both groups received the same initial treatment with rituximab. Five year OS rate in group 1 was significantly higher than in group 2 (83±7% vs 28±13%; ð=0.03). In all 59 cases the samples for IHC analysis were selected by using a table of random numbers, without knowing to which study group they belonged. Each study parameter (microvessel density, number of cytotoxic lymphocytes and macrophages within a tumor) was evaluated and then assigned to prognostic group 1 or 2.
The vascularization of tumor tissue was assessed by IHC on sections from paraffin blocks of tumor lymph node biopsies. CD34 and D2-40 (podoplanin) antibodies were used for the visualization of blood and lymphatic vessels, respectively. CD68 antibody was used to detect activated macrophages. Granzyme B antibody was used to visualize cytotoxic lymphocytes.
Morphometric analysis was performed using light microscopy and a Leica digital camera (400x). The pictures were processed by the computer program “VideoTesT-Morphology 5.2” in order to estimate the percentage of vessels in the tumor tissue. IHC specimen evaluation was carried out using a table of random numbers. Number of macrophages and cytotoxic lymphocytes in nodular and nodular-diffuse types of tumor growth was evaluated by light microscopy (400x): the cells were counted in 1 mm2 of tumor tissue, and the number of positive cells was determined in the intrafollicular and interfollicular space.
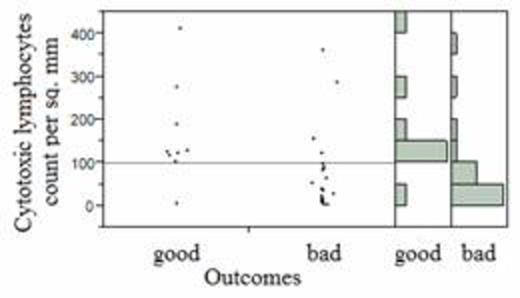
Blood vessel density and lymph vessel density in group 2 were significantly higher than in group 1 (p=0.03). The cut-off point for blood and lymphatic vessel density in 1 mm2, which differentiates group 1 from group 2, was 0.04. The number of cytotoxic lymphocytes in intrafollicular space, interfollicular space and diffuse area of tumor nodules in group 1 was significantly higher than in group 2 (ð=0.05). The cut-off point for tumor-associated cytotoxic lymphocytes in 1 mm2, which differentiates group 1 from group 2, was 100 (Figure 1). The number of macrophages within tumors with nodular and diffuse growth in group 2 was significantly higher than in group 1 (ð=0.01) (Figure 2). The cut-off point for macrophages in 1 mm2, which differentiates group 1 from group 2, was 250. Statistical analysis were done using JMP ver. 10.0 (SAS, Cary, NC).
Our results demonstrate an association between higher angiogenic activity in the tumor and poor prognosis. A low number of cytotoxic lymphocytes and a high number of macrophages within the tumor were also associated with a poor prognosis. We suggest that these results will help to predict clinical response in FL using rituximab.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.


This feature is available to Subscribers Only
Sign In or Create an Account Close Modal