Abstract
The incidence of obesity is increasing worldwide and is associated with numerous adverse health outcomes. Obesity was associated with more toxicity and worse prognosis in pediatric AML patients. On the other hand diabetic patients diagnosed with AML have multiple complications related to infection organ failure and chemotherapy side effects, Previous epidemiological studies in children have shown significant correlations in incidence between AML and DM in children.
To study Body-Mass Index (BMI) and uncontrolled DM impact on clinical outcome of adult AML pts.
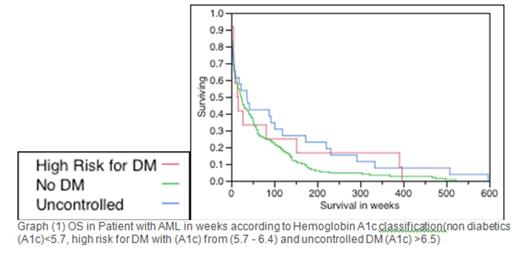
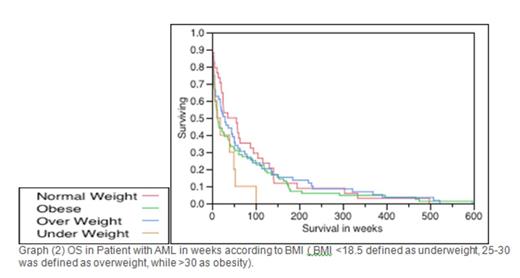
A total of 187 adult pts with AML between 2002-2011 were enrolled. Retrospective data included demographics, labs, cytogenetics and outcome. LeukemiaNET Standardization (LNS), complete remission (CR), overall survival (OS) and relapse free survival (RFS) were obtained (Dohner E, Blood 2010). BMI of <18.5 defined as underweight, 25-30 was defined as overweight, while >30 as obesity. On the other hand Fasting blood glucose and Hemoglobin A1c were measured, DM severity was classified according to guidelines, as non diabetics (A1c)<5.7 and normal FBG<100, high risk for DM with (A1c) from (5.7 - 6.4) and uncontrolled DM (A1c) >6.5. Fischer's and Wilcoxon tests were used for comparatives between groups, cox proportional hazards and logistic regression for associations for OS/RFS and CR, Kaplan-Meier test for OS and RFS estimates via JMP software V9.0. IRB approval was obtained according to Helsinki declaration.
The median age was 70 years, with 98 (52%) were men. 45 pts (24%) had complex cytogenetics, 28 pts (15%) had AML progressed from MDS. Median BMI was 28.7 (range 14.8-51.4). 10 (5%) were underweight, 34 (18%) had normal BMI, 59 (32%) were overweight, and 84 (45%) were obese. 149 pts (80%) were not Diabetic, 12 pts (6%) had high risk for DM, 26 pts (14%) uncontrolled DM. Overall Median OS was 23 weeks; 46 weeks in normal BMI, 30 weeks in overweight, 14 weeks in obese, 15 weeks in underweight, A according to DM subgroups; 24 weeks non-diabetics, 15 weeks had high risk for DM, 37 had uncontrolled DM. At diagnosis, BMI or Hemoglobin A1c classes were not associated with age, sex, white blood count (WBC), platelets, blasts, ECOG status, LNS; nor treatment toxicities. Even though median survival in weeks was lower in obese and underweight pts, Median OS and RFS were not different in univariate or across BMI subgroups (p=0.32 and 0.22) or Hemoglobin A1c subgroups (p=0.19 and 0.71)
BMI and uncontrolled DM did not show statistically significant correlation with LNS, relapse rates, OS or RFS.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal