Abstract
CD36 is a marker that typically occurs on monocytes and erythroid cells, but may rarely occur on the leukemic blasts in childhood B-lymphoblastic leukemia (B-LL). We have observed that our B-LL patients whose blasts are CD36+ often have cytoplasmic granules. B-LL blasts with cytoplasmic granules are a rare finding seen in only 2-7% of children. Some previous studies have suggested that granular blasts are associated with worse prognosis, while other studies did not observe this relationship. Because our patients with CD36+ blasts, with or without cytoplasmic granules, seemed to have a relatively poor prognosis, we set out to describe the patient, disease, molecular/cytogenetic, and treatment response characteristics of these patients. We hypothesized that they would have a significantly decreased event free survival (EFS) and overall survival (OS) compared to standard risk patients.
We performed an IRB approved retrospective review of all flow cytometry reports from September 2008 until April 2013. Diagnostic marrow flow reports and slides were obtained for each patient reported to have blasts expressing CD36. Patients were deemed eligible if they had a marrow aspirate at initial diagnosis demonstrating moderately bright CD36 expression on at least 5% of the leukemic blasts. We abstracted data on patients, disease (including the presence of granules), and treatment characteristics from patients' charts. We estimated EFS (induction failure, relapse, or death) and OS, using the Kaplan-Meier method.
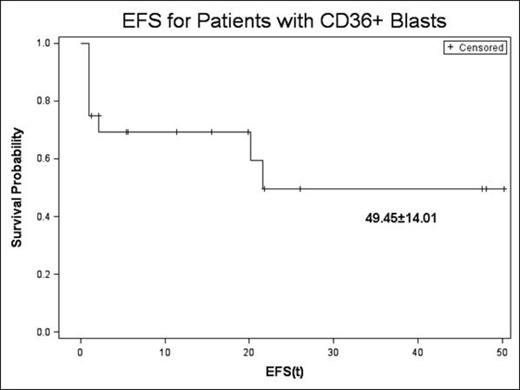
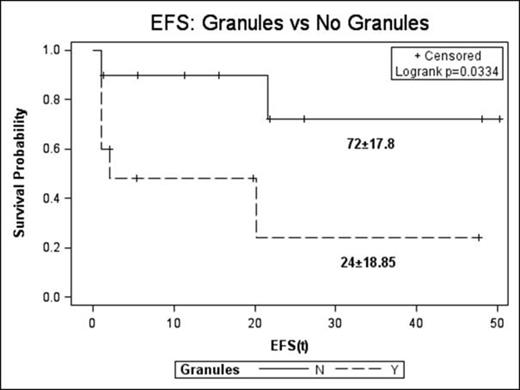
We identified 20 cases of CD36+ B-LL. Fourteen of the patients were male. Ten were Hispanic, 6 were White, 3 were African American, and one was Pakistani. Two had Down's syndrome. Eleven patients were <10 years old and 15 had a WBC count at diagnosis <50x109/liter. Eleven patients were classified as NCI high risk by age or WBC count. Two patients had CNS disease and none had testicular disease. Eleven patients had cytogenetic abnormalities, but only 5 had risk defining abnormalities (1 double trisomy 4 and 10, 1 iAMP21, 3 Ph+). The mean blast expression of CD36 was 26.92% (+/-19.22). In 10 cases, the leukemic blasts had cytoplasmic granules. In 14 cases the blasts expressed CD10 and in 13 they expressed at least 1 myeloid marker (CD13, CD33, CD15, CD64, or CD117). Patients were treated on a variety of protocols, depending on risk classification at diagnosis and the opportunity for study enrollment. In 15 cases there was a suboptimal response to induction: 5 failed induction and 10 had minimal residual disease (≥0.01%) at day 29 of induction. Five patients underwent hematopoietic stem cell transplant – 4 in 1st complete remission and 1 in 2nd complete remission. With a median length of follow up of 21.56 months, 3-year EFS was 49.45±14.01 (Fig 1); for patients whose blasts did not have granules it was 72±17.8 but for those whose blasts did have granules it was 24±18.85 (p=0.033) (Fig 2). Three-year OS was 75±12.83.
3-year EFS for the entire study cohort.
3-year EFS for patients with no cytoplasmic granules vs with granules.
3-year EFS for patients with no cytoplasmic granules vs with granules.
Our results suggest that in pediatric patients with B-LL, the combination of CD36 expression and cytoplasmic granules is associated with a poor prognosis. This finding needs to be confirmed in a larger sample, using multivariate analysis to assess the contribution of these two factors with respect to established risk factors. Future studies should also examine the gene expression profile of these leukemias to determine whether there are distinctive molecular abnormalities that may account for the poor prognosis.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal