High dose chemo/radiotherapy with autologous hematopoietic cell transplantation (HCT) has been shown to be an effective therapy for a variety of malignancies. However, as more patients survive both the disease and the early post HCT period, it has become apparent that other potential long term complications, mainly secondary malignancies may hamper patients' prospects.
We analyzed the incidence of different secondary malignancies occurring after consolidation with autologous HCT compared to other modalities for the treatment of various hematological and non-hematological malignancies.
Systematic review and meta-analysis of randomized controlled trials comparing high dose therapy with autologous HCT to other treatment modalities (observation, immunotherapy or chemotherapy). We searched the Cochrane Library, MEDLINE and conference proceedings. Outcomes assessed were rates of AML/MDS, solid tumors and overall secondary malignancies. Relative risks (RR) with 95% confidence intervals (CIs) were estimated and pooled. Heterogeneity is given when approporiate.
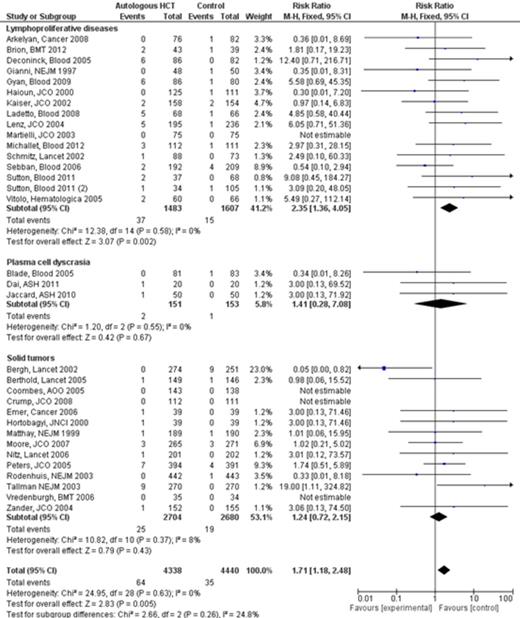
Our search yielded 74 trials fulfilling inclusion criteria; among them 38 trials recruiting 10131 patients reporting secondary malignancies were included. Baseline diseases were lymphoproliferative diseases (n=17), plasma cell dyscrasias [PCD] (n=5) and solid tumors (n=16). The studies were conducted between the years 1987 and 2007. Median follow up was 55 (range 12-144) months. High dose therapy consisted of variety of regimens. Comparative arm regimens were either observation (n= 6), intensive chemotherapy [>6 gr/m2 of cyclophosphamide or high doses of etoposide] (n= 6), or standard chemotherapy (n= 24). Overall, the RR for secondary malignancies was 1.25 (95% CI 0.99-1.57) (38 studies, 10131 pts). Among all patients, there was a higher rate of MDS/AML in patients given HCT compared to other treatments [RR=1.71 (95% CI 1.18-2.48)], (33 studies, 8778 patients), Figure. Subgroup analysis showed similar results in patients with lymphoproliferative diseases [RR=2.35 (95% CI 1.36-4.05), (16 studies, 3090 patients)]. However, the rate of AML/MDS was not increased in patients treated for PCD or solid malignancies [RR=1.41 (95% CI 0.28-7.08), 3 studies, 304 patients and RR=1.24 (95% CI 0.72-2.15), 14 studies, 5384 pts, respectively], Figure. Subgroup analysis based on the comparator's intensity- showed a higher rate of MDS/AML merely in patients given HCT compared to observation and to low intensity [RR=4.86 (95% CI 1.43-16.47), (5 studies, 732 patients) and RR=2.09 (95% CI 1.30-3.35), (19 studies, 6036 patients)]. Overall, there was no difference in the rate of secondary solid malignancies between patients given HCT and patients given other treatments [RR=0.95 (95% CI 0.67-1.32), (19 studies, 5925 patients)], with similar results in subgroup analysis according to the baseline diseases.
The rate of secondary MDS/AML is higher in patients given high dose therapy and autologous HCT compared to other treatment options, with statistically significant higher rates only in the subgroup of patients with lymphoproliferative diseases. The rate of secondary solid malignancies is similar among all patients given either high dose therapy or alternative therapy.
No relevant conflicts of interest to declare.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal