The aim of this registry-based retrospective study was to analyze the outcome of second alloSCT (alloSCT2) performed in patients with malignant lymphoma who had relapsed after a first alloSCT (alloSCT1).Another purpose was to identify prognostic factors which might influence outcome after alloSCT2.
Primary endpoint was disease-free survival (DFS) measured from alloSCT2; secondary endpoints were overall survival (OS), non-relapse mortality (NRM), and incidence of relapse (REL).
Eligible were patients >=18 years who were registered within the EBMT and had received an alloSCT2 for relapse of lymphoma between 2000-2011 with a minimum interval of 3 months between alloSCT1 and alloSCT2. Centers with eligible patients were contacted to provide additional treatment and follow-up information.
Statistical analysis was descriptive and employed log rank comparisons for univariate assessment of the impact of baseline characteristics on survival endpoints.
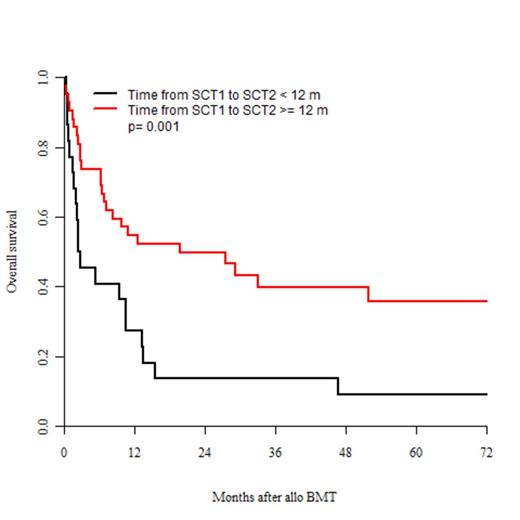
229 patients were identified who fulfilled the inclusion criteria. Additional information upon center request was provided for 84 them, resulting in exclusion of 19 patients who had been re-grafted for reasons other than relapse. The final study sample of 65 patients had a median age of 39 (18-67) years, a median interval from diagnosis to alloSCT1 of 21 (4-107) months, and a median interval from alloSCT1 to alloSCT2 of 18 (3-169) months. Diagnosis was Hodgkin's lymphoma (HL) in 29%, diffuse large B cell lymphoma (DLCL) in 14%, T cell lymphoma (TCL) in 12%, lymphoblastic lymphoma in 12%, follicular lymphoma (FL) in 11%, mantle cell lymphoma (MCL) in 11%, and other lymphoma in 11% of the patients. Remission status at alloSCT2 was CR/PR in 28% and more advanced in 72%. The same donor was used in 55% of the second allotransplants, whereas an alternative donor was used in 45%. Conditioning was myeloablative in 32% and less intensive in 68% of the alloSCT2 procedures. With a median observation time after alloSCT2 of 73 (13-73) months, DFS, OS, REL, and NRM were 26%, 37%, 55%, and 19% at 2 years; and 19%, 27%, 61%, and 19% at 5 years after alloSCT2. 45 patients died (26 from relapse and 19 from other reasons, mainly multi organ failure due to GVHD, infectious complications or toxicity). 15% of the patients suffered from grade 3/4 acute GVHD. The cumulative incidence of chronic GVHD was 34% at 2 years. Whilst DFS and OS were adversely affected by non-remission at alloSCT2 (p=0.017 and p=0.004) and interval between alloSCT1 and alloSCT2<12 months (p=0.011 and p=0.001; Fig. 1), underlying diagnosis (HL vs. DLCL/FL/MCL vs. TCL) and donor (same vs. alternative donor) had no significant impact.
Although disease recurrence remains a problem, second allogeneic transplantation is a reasonable option in patients with lymphoma relapse after a first allogeneic transplantation, resulting in long-term remission in a substantial proportion of patients – in particular if the interval between alloSCT1 and alloSCT2 is 12 months or longer.
OS after BMT depending on interval between alloSCT1 and alloSCT2 (</>= 12 months)
No relevant conflicts of interest to declare.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal