Chronic graft versus host disease (GVHD) affecting eye and mouth are common complications of allogeneic hematopoietic stem cell transplantation (HCT). Although not life threatening, these forms of chronic GVHD are associated with significant morbidity and are difficult to treat. The risk factors associated with the development of chronic eye and mouth GVHD in unrelated donor transplantation (URD-HCT) are unknown. In order to identify risk factors for these two forms of organ specific GVHD we performed a retrospective review of patients who underwent URD-HCT at Princess Margaret Cancer Center, Toronto, Canada between January 2002 and October 2012.
During this period 280 patients underwent URD-HCT. The median age was 47 (range 18-71) years and 58% were males. Disease indications for HCT were acute myeloid leukemia or myelodysplastic syndrome (54%), acute lymphoblastic leukemia (15%), chronic myeloid leukemia (10%), lymphoma (8%), myelofibrosis (6%), chronic lymphocytic leukemia (4%) and others (3%). Forty six (16%) patients had single antigen or allele mismatched donors. Graft source was peripheral blood stem cells in 212 (76%) patients and bone marrow in 68 (24%). One hundred eighty eight patients (67%) had full intensity conditioning and 92 (33%) had reduced intensity. GVHD prophylaxis consisted of cyclosporin (CSA) in 31%, CSA with methotrexate (MTX) in 29% and CSA with mycophenolate mofetil (MMF) in 40%. Forty six percent of patients received in vivo T- cell depletion (TCD) with alemtuzumab in addition to CSA-based GVHD prophylaxis.
At a median follow up of 30 months (range, 1-134), 136 (49%) patients had developed chronic GVHD. Fifty eight (21%) patients had developed manifestations in eyes and 82 (29%) in mouth. In multivariable analysis no clinical variables were found to be predictive of overall chronic GVHD.
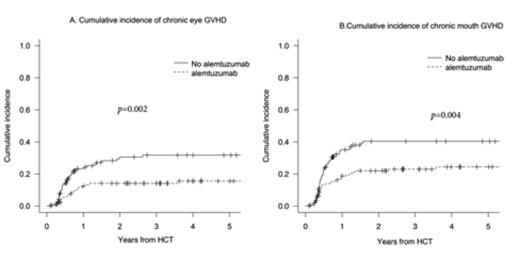
In multivariable analysis TCD was the only predictive factor for chronic eye GVHD (HR=0.46; 95% CI, 0.27-0.79, p=0.005). The 5-year cumulative incidence of chronic eye GVHD in the TCD group was 16% vs. 32% in the non-TCD group (p= 0.002) (Figure 1A).
Figure 1
TCD was not a significant covariable for chronic skin, liver or gut GVHD. Prior grade 2-4 acute GVHD was the only predictive factor for skin and gut involvement and there was no predictive factor was identified for liver involvement. However TCD along with recipient age and source of stem cell was a significant covariable for lung GVHD. There was no difference in 5-year overall survival between the non-TCD and the TCD groups (45% vs. 36 %, p=0.4).
These data suggest that TCD is associated with reduced incidence of chronic eye and mouth GVHD in URD-HCT without any significant effect on overall survival. It appears that risk factors for the development of organ-specific GVHD may vary based on the organ of involvement.
No relevant conflicts of interest to declare.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal