It has been previously reported that increased fluid accumulation during peripheral blood hematopoietic stem cell (HSC) mobilization is associated with poor outcome in patients with amyloidosis who undergo autologous HSCT. It is unknown whether increased fluid accumulation during the early phases of HSCT is associated with poor survival in patients undergoing HSCT for other diseases.
To determine the impact of fluid accumulation during conditioning and in the first 10 days post HSC infusion on survival and risk of complications of patients who underwent both autologous and allogeneic HSCT.
We retrospectively reviewed the medical charts of 257 consecutive patients who underwent HSCT at our institution from January, 2007 until December, 2012. Information on patients' body weight (BW) was measured daily, starting at admission. The highest BW recorded until HSC infusion (D0) and until the first 10 days post-SCT (D+10) was used to calculate the BW increase in relation to the baseline BW. A ROC curve was built to determine the best cut-off point in BW increase that predicted for mortality. Information on the incidence of post-transplant complications was extracted from the time period that patients were admitted for transplant until discharge from the hospital. Endpoints analyzed included the presence or absence of respiratory failure, acute renal failure, sinusoidal obstruction syndrome (SOS), septic shock and requirement of diuretic use, hemodialysis, mechanical ventilation and ICU admission. Overall survival (OS) was estimated from the time of HSCT until death, and surviving patients were censored at last follow-up. Variables entered into the multivariate Cox analysis were those with a p-value<0.10 in the univariate analysis. Statistical analysis was performed with STATA (v11.0) and alfa error was defined as 5%.
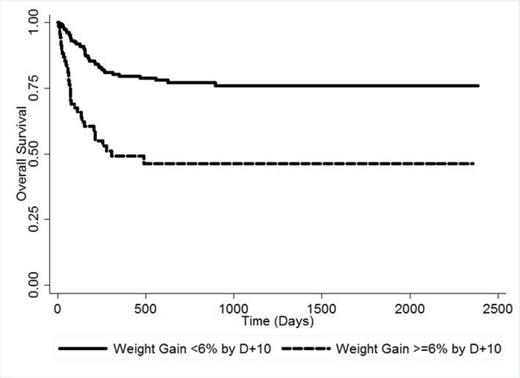
Mean age was 39.4 years old (range <1 year-76 years) and 61% were male. HSC sources included autologous (47%), matched related donors (15%), matched unrelated donors (13%), cord blood units (19%) and mismatched related/unrelated donors (6%). Diagnosis included acute leukemia or chronic myeloid disorders (37%), lymphoma/multiple myeloma (42%) and non-malignant hematological disorders (21%).The results of the ROC curve defined the cut-point of 6% BW gain by D+10 as the best predictor for OS. A total of 69 patients (27%) had a BW increase ≥6% by D+10. This was associated with an increased risk of mortality, with a 100-days OS of 67% vs. 92% (HR 3.25, p<0.0001, 95% CI 2.04-5.18; Figure). A greater than 6% gain in BW by D+10 was also associated with an increased risk of developing SOS (31% vs. 6%; p<0.0001), septic shock (29% vs. 7%; p<0.0001), respiratory failure (35% vs. 9%; p<0.0001) and requiring diuretic use (91% vs. 71%; p<0.001), hemodialysis (13% vs. 4%, p=0.007), mechanical ventilation (33% vs. 9%; p<0.0001) and ICU admission (42% vs. 24%; p<0.0001). In a multivariate analysis considering age, diagnosis, type of SCT and sex, a ≥6% BW gain by D+10 was an independent variable associated with an increased risk of mortality (HR 3.28; p<0.0001; 95% CI 2.02-5.32). We next evaluated the prognostic impact of a ≥6% BW increase in the time period from admission until D0. Our results showed that it was similarly associated with an increased risk of mortality (HR 2.26; p=0.003; 95% CI 1.32-3.86), of developing SOS (32% vs. 9%; p<0.0001), respiratory failure (27%vs. 14%; p=0.04) and requiring hemodialysis (15% vs. 5%; p=0.01) and ICU admission (37% vs. 18%; p=0.008). After adjusting for age, sex, diagnosis and type of SCT, ≥6% BW gain by D0 was associated with an increased mortality (HR 1.94; p=0.026; 95% CI 1.08-3.48).
In our cohort of patients, fluid accumulation during the early stages of conditioning regimen and HSCT, reflected by a ≥6% increase in BW, was associated with an increased mortality and risk of developing severe complications. This may reflect the presence of increased endothelial damage, and further studies are needed to better clarify the mechanism behind weight gain during HSCT. Our results demonstrate that patients who have a ≥ 6% gain in BW by D0 and D+10 have an increased risk of complications, and more intensive monitoring of these patients is needed.
No relevant conflicts of interest to declare.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal