The effect of CMV reactivation after allo-HCT on relapse and overall survival (OS) in patients with acute myeloid leukemia (AML) and myelodysplatic syndrome (MDS) is controversial (Green et al blood 2013, Elmaagacli et al Blood 2011, and Erard et al Hematologica 2006).
We retrospectively analyzed the effect of CMV reactivation on OS and cumulative incidence of relapse (CIR) and non-relapse mortality (NRM) in AML and MDS patients older than > 18 years who had received allo-HCT between 2005-2011 and had not died within 30 days of receiving allo-HCT at MD Anderson Cancer Center. The effect of any CMV antigenemia on allo-HCT outcomes was evaluated by comparing any CMV antigenemia with no CMV antigenemia. Because of potential immunomodulatory effect of CMV infection, the effect of prolonged antigenemia (defined as CMV antigenemia with duration more than 12 days, the median duration of antigenemia for the cohort) on transplant outcomes was analyzed by comparing patients with prolonged antigenemia with patients with no CMV antigenemia or CMV antigenemia with ≤ 12 days. All patients underwent surveillance by pp65 antigenemia test. Preemtive therapy was initiated for > 3 pp65 Ag cells/million WBC's. Kaplan-Meier survival curves were used to estimate OS and the log-rank test was used to assess group differences. CIR and NRM were determined using the competing risks method; competing risk for CIR was death and for NRM was relapse. Group differences in CIR and NRM were assessed using Gray's test.
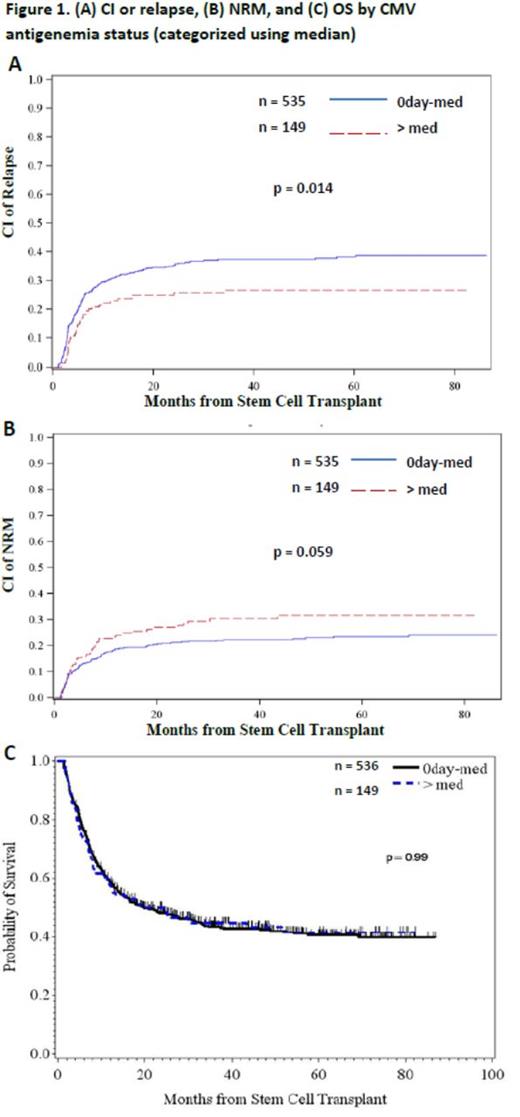
Table 1 shows baseline characteristics. Comparing R+/D+, R-/D-, R-/D+, and R+/D- groups, the incidence of any CMV antigenemia after HCT was 48%, 16.7%, 13.5%, and 50.9%, respectively (p<0.0001) and the incidence of CMV disease was 1.0%, 1.9%, 2.7%, and 4.5%, respectively (p = 0.05). When any CMV antigenemia was compared with no CMV antigenemia post allo-HCT, CMV reactivation had no effect on OS (p > 0.15) and CIR (p > 0.61) in all cohort as well as AML and MDS subgroups. Comparing any antigenemia vs. no antigenemia, CIR at 3 years was 34.6% vs. 35.2% in all cohort, 36.7% vs. 36.6% in AML patients, and 29.5% vs. 30.0% in MDS patients, respectively. In patients with CMV antigenemia, duration of antigenemia ranged from 1 to 535 days (median 12 days). We then investigated the effect of prolonged CMV antigenemia on transplant outcomes. Patients with CMV antigenemia > 12 days compared with combined group of ≤ 12 days or no CMV antigenemia had a lower cumulative incidence of relapse and a higher NRM, resulting in a similar OS (Fig. 1). Such a difference was seen in AML but not in MDS subgroup. We then investigated the effect of duration of CMV antigenemia in patients with CMV reactivation. Comparing 1-12 days of antigenemia vs. more than 12 days of antigenemia, CIR at 3 years was 41.9% vs. 26.7% (p = 0.003) in all cohort, 45.8% vs. 26.4% (p = 0.001) in AML patients, and 32.1% vs. 27.4% (p = 0.68) in MDS patients, respectively.
Patients characteristics
| Measure . | All Patients N (%) . |
|---|---|
| Disease subtype, n (%) | |
| AML | 524 (76) |
| MDS | 161(24) |
| Age at SCT (years) | |
| Mean | 52.8 |
| Transplant type, n (%) | |
| MRD | 310 (45.3) |
| MUD | 317 (46.3) |
| 1 AG MMUD | 50 (7.3) |
| 2 AG MMUD | 1 (0.1) |
| 1 AG MMRD | 5 (0.7) |
| 2 AG MMRD | 1 (0.1) |
| SYNG | 1 (0.1) |
| HLA DP match status, n (%) | |
| Yes | 379 (55.3) |
| No | 306 (44.7) |
| Conditioning regimen, n (%) | |
| Myeloablative | 552 (80.6) |
| CMV risk groups, n (%) | |
| D+/R+ | 294 (43.6) |
| D-/R- | 54 (8.0) |
| D+/R- | 37 (5.5) |
| D-/R+ | 289 (42.9) |
| Missing | 11 |
| Disease risk, n (%) | |
| Low | 36 (5.3) |
| Intermediate | 203 (29.8) |
| Intermediate-1 | 48 (7.0) |
| Intermediate-2 | 56 (8.2) |
| High | 338 (49.6) |
| Missing | 4 |
| Disease status at transplant, n (%) | |
| Complete remission | 374 (54.6) |
| Refractory | 232 (33.9) |
| Untreated | 77 (11.2) |
| Unknown | 2 (0.2) |
| Measure . | All Patients N (%) . |
|---|---|
| Disease subtype, n (%) | |
| AML | 524 (76) |
| MDS | 161(24) |
| Age at SCT (years) | |
| Mean | 52.8 |
| Transplant type, n (%) | |
| MRD | 310 (45.3) |
| MUD | 317 (46.3) |
| 1 AG MMUD | 50 (7.3) |
| 2 AG MMUD | 1 (0.1) |
| 1 AG MMRD | 5 (0.7) |
| 2 AG MMRD | 1 (0.1) |
| SYNG | 1 (0.1) |
| HLA DP match status, n (%) | |
| Yes | 379 (55.3) |
| No | 306 (44.7) |
| Conditioning regimen, n (%) | |
| Myeloablative | 552 (80.6) |
| CMV risk groups, n (%) | |
| D+/R+ | 294 (43.6) |
| D-/R- | 54 (8.0) |
| D+/R- | 37 (5.5) |
| D-/R+ | 289 (42.9) |
| Missing | 11 |
| Disease risk, n (%) | |
| Low | 36 (5.3) |
| Intermediate | 203 (29.8) |
| Intermediate-1 | 48 (7.0) |
| Intermediate-2 | 56 (8.2) |
| High | 338 (49.6) |
| Missing | 4 |
| Disease status at transplant, n (%) | |
| Complete remission | 374 (54.6) |
| Refractory | 232 (33.9) |
| Untreated | 77 (11.2) |
| Unknown | 2 (0.2) |
Prolonged CMV antigenemia is associated with decreased relapse in patients with AML, but not in MDS. Lower relapse is offset by increased NRM resulting in no change in OS. In contrast with published data, lower rate of relapse was not found when any antigenemia was compared with no antigenemia.
No relevant conflicts of interest to declare.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal