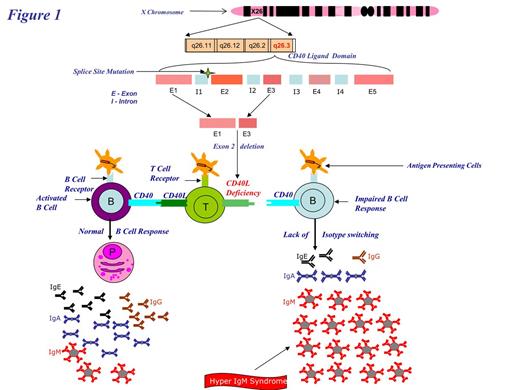
Pre-Implantation genetic diagnosis and pre implantation Human Leukocyte Antigen (HLA) typing has been successfully used to conceive unaffected HLA identical siblings to provide stem cells for Hematopoietic Stem Cell Transplant (HSCT) (Goussetis, Evgenios, et al. Biology of Blood and Marrow Transplantation 16.3 (2010): 344-349). This technique has been effective in treatment of disease such as Leukemia, Diamond-Blackfan anemia, Thallasemia etc. With improvement of molecular techniques it has been possible to do gene testing from a single cell. We report first case of X-linked Hyper CD40 ligand deficiency where preimplantation genetic diagnosis (PGD) and pre implantation HLA typing were used to achieve successful HSCT from the resulting HLA identical sibling donor. We used dual hematopoietic stem cell sources from cord blood and bone from the nine month old sibling. Currently, patient is 34 months post transplantation doing well with full immunologic reconstitution.
The repeat tests confirmed that the proposed donor baby was unaffected and a 10 of 10 HLA match for the patient. The patient was subjected to a conditioning regimen consisting of Busulfan, Cytoxan and GVH prophylaxis with Methotrexate and Tacrolimus. Following the regimen, the patient was infused with stem cell dose consisting of fresh bone marrow (1.86x108 TNC/Kg) harvested from the matched sibling donor and cryopreserved cord blood (0.29x108 TNC/Kg) obtained during the sibling donor's birth. The patient was found to be well engrafted (98% on day 18, 100% at 9 months) post transplant. The CD40L test showed 60% CD40L on T cells after stimulation with ICOS (inducible co-stimulator) increased from 0% pre-transplant.
Most patients with hyper CD40 ligand deficiency inherit the causative gene mutation from one of their parents. The average family size in the US is 3.14 (Daphne Lofquist, et al. Households and Families: 2010 Census Briefs).This results in a low probability of finding a sibling donor that is both unaffected and a HLA match. Undergoing multiple pregnancies with low probabilities of conceiving an unaffected HLA matched sibling is stressful, time consuming and ineffective. PGD combined with HLA typing provides an effective way of choosing an embryo that result in a matched HLA donor sibling and subsequent successful stem cell transplant.
No relevant conflicts of interest to declare.


This feature is available to Subscribers Only
Sign In or Create an Account Close Modal