The therapeutic potential of allogeneic hematopoietic stem cell transplantation (HSCT) mainly relies on graft-versus-leukemia effects mediated by donor-derived T cells targeting both minor histocompatibility antigens and tumor-associated antigens (TAAs). The efficacy of TAA-mediated immune responses particularly depends on the level of antigen expression in the target tissue and the presence of a proinflammatory immune environment allowing donor-derived T cells to overcome peripheral tolerance and to attack the malignant cells in a selective manner. As several TAAs with clinical relevance in tumor and/or transplant immunotherapy such as Mucin 1 (MUC-1), Preferentially expressed antigen of melanoma (PRAME), Wilms tumor protein 1 (WT1) and Human epidermal growth factor receptor 2 (HER2/neu) are highly expressed in the placental tissue we investigated the effects of pregnancy on the frequency of immune responses against these TAAs in a prospective study. A cross-sectional analysis in a previously reported group of 114 healthy volunteer blood donors revealed no significant effects of prior pregnancies. Here, we present the results of the longitudinal analysis in women during and after their first pregnancy.
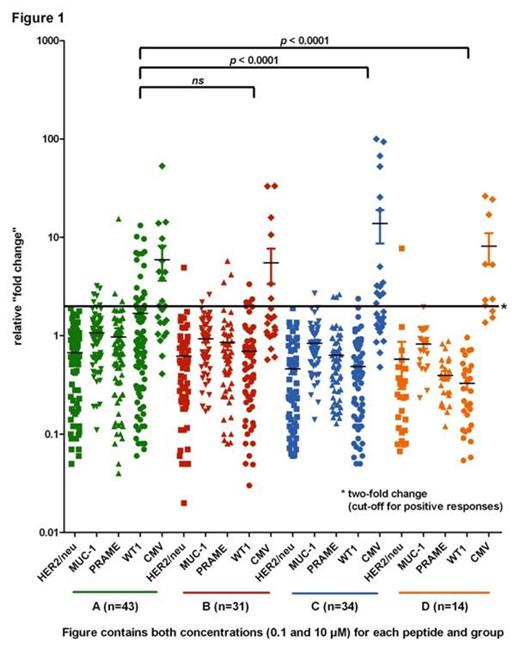
After local ethical approval and written informed consent a total of 44 HLA-A*02:01-positive women during their first pregnancy were enrolled in this prospective study. Immune responses against TAAs were assessed at four different time points: First or second trimester (Time point A, n=43), 1 to 3 days after delivery (Time point B, n=31), 6 to 8 weeks after delivery (Time point C, n=34) and after completed nursing (Time point D, n=14). At each time point peripheral blood was drawn and peripheral blood mononuclear cells (PBMCs) were collected by density gradient centrifugation. Isolated CD8+ T cells were stimulated with irradiated T2 cells which were loaded with immunodominant peptides (0.1 and 10 µM) of HER2/neu, MUC-1, PRAME, and WT1. Interferon-gamma (IFN-γ) mRNA expression was measured by quantitative polymerase chain reaction (qPCR) after extraction of total RNA. IFN-γ mRNA expression was calculated as relative fold change compared to the irrelevant melanoma antigen Glycoprotein 100 (gp100). A two-fold change was considered as cut-off for positive results. A HLA-A*02:01 restricted CMV peptide was used as positive control.
All results are presented in Figure 1. Positive immune responses are presented above the cut-off line. A significant number of positive immune responses against MUC-1, PRAME and WT1 were found during pregnancy (Group A) and early after delivery (Group B). The frequency of positive immune responses against these TAAs decreased during and/or after the period of nursing leaving only one borderline significant finding behind (Group C and D). Against HER2/neu there were none or only single events of immune responses detectable in any group.
The results from this longitudinal analysis show that immune responses against the transplant-relevant TAAs MUC-1, PRAME and WT1 are detectable in pregnant women but are lost after delivery. These findings are in line with our observations from the inter-individual cross-sectional study where women with prior pregnancy did not have a significantly increased frequency of immune responses against TAAs compared to women without prior pregnancies. The abrogation of the immune response as shown in a longitudinal manner is likely to be a result of an immunosuppressive environment induced by increasing levels of steroid hormones during pregnancy. As immune responses against TAAs can be found also in non-pregnant women we assume that the overexpression of TAAs in the placenta induces a boost in autoimmune responses that is consequently compromised by the immunosuppressive environment. Therefore pregnancy may be a useful model for the boost and the regulation of immune responses against TAAs with implications for immunotherapy.
No relevant conflicts of interest to declare.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal