Abstract
Human immunodeficiency virus (HIV) infected individuals have an increased incidence of malignancies, including B-cell lymphomas. The use of highly active antiretroviral therapy (HAART) during antineoplastic therapy for HIV related lymphoma remains controversial. The current meta-analysis investigates the impact of the upfront addition of HAART to chemotherapy on overall survival (OS) compared to chemotherapy alone.
We searched MEDLINE (January 1996 to May 2013), the Cochrane Central Register of Controlled Trials (May 2013), and the references of retrieved articles. Published clinical trials were included that both clearly defined the patients treated with and without HAART and provided the respective outcomes for each group. Two authors independently assessed the quality of studies and abstracted data. Primary outcomes were complete remission (CR) and overall survival (OS). Hazard ratios were pooled using random effects methods. Heterogeneity was assessed with I2 and by visual inspection of the Galbraith plots. Sources of heterogeneity were explored using stratified analysis and random-effects meta-regression.
Four retrospective chart reviews, one retrospective case control, two cohort studies, one randomized trial, and two prospective trials were eligible for review, providing 1070 subjects with an average age of 41.3 years. The mean CD4 count was 223/μl and HIV viral load 192,452 copies/ml. There was significant heterogeneity between studies.
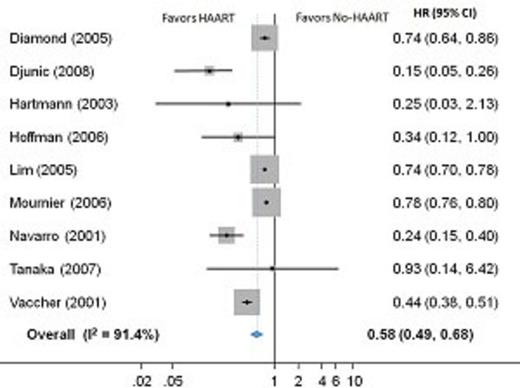
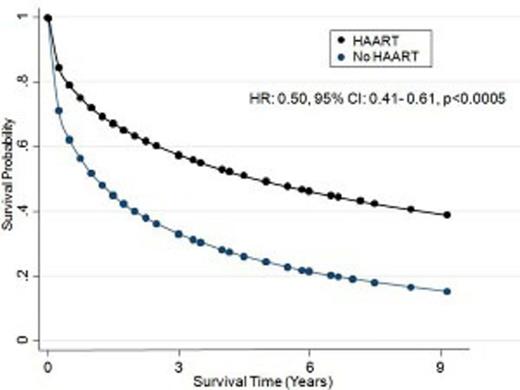
Individuals receiving HAART were more likely to achieve CR compared to those not receiving HAART (RR 1.47, CI: 1.04-2.06, I2=75.0%). Among those receiving HAART, 56% (95% CI: 45%-67%, I2=67.8%) achieved CR compared to 37% (95% CI: 28%-45%, I2=75.1) not receiving HAART. The addition of HAART to chemotherapy improves OS when compared to those receiving chemotherapy alone (HR: 0.58, 95% CI: 0.49-0.68, I2=91.4%, Figure 1), representing an increased median OS time of 20.5 months (95% CI: 2.6-38.4, I2=93.6%). Calculation of a pooled HR using survival curve data from studies with extractable data yielded similar results (HR: 0.50, 95% CI: 0.41-0.61, Figure 2). Higher CD4 counts were associated with improved survival (p<0.0005). Conversely, older age (p=0.017), higher viral load (p<0.0005), higher stage lymphoma (p=0.023), the presence of B-symptoms (p<0.0005), and worse functional status (p<0.0005) were associated with decreased survival. Following adjustment for these predictors, concurrent HAART and chemotherapy resulted in improved OS (HR: 0.46, 95% CI: 0.38-0.57). There was no evidence of publication bias for any of our outcomes (CR: p=0.39, median survival: p=0.47, HR: p=0.07). There was also no relationship between quality and any of our outcomes (CR: p=0.77, median survival: p=0.32, HR: p=0.33).
Overall survival comparing chemotherapy concurrent with or without HAART.
Pooled overall survival analysis curve from regression model comparing chemotherapy concurrent with or without HAART.
Pooled overall survival analysis curve from regression model comparing chemotherapy concurrent with or without HAART.
Overall survival and complete remission are improved with the upfront addition of HAART to chemotherapy when compared to chemotherapy alone for patients with HIV related B-cell lymphoma.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal