Abstract
Primary central nervous system lymphoma (PCNSL) is a rare form of extranodal non Hodgkin lymphoma, accounting for approximately 3-4% of new primary brain tumors and approximately 1% of all NHL. The overall incidence of PCNSL is approximately 0.43/100,000 per year, but the relative risk of disease among immunocompromised patients is considerably higher; approximately 3600 times that of the general population. Similarly, the average age of onset, race, treatment regimens and overall survival are all markedly different amongst immunocompetent and immunocompromised patients with PCNSL. The standard treatment for immunocompetent includes high-dose methotrexate based regimens with or without whole brain radiation therapy (WBRT). On the contrary, there is little to no prospective data guiding the treatment of immunocompromised patients with PCNSL. The standard therapy for these patients has yet to be defined, leaving the majority to receive the potentially sub-optimal regimens including WBRT in addition to highly active antiretroviral therapy (HAART). The current study reports on survival data from a retrospective cohort of patients with biopsy-proven PCNSL diagnosed at our institution over the last decade stratified by both HIV status and therapy received.
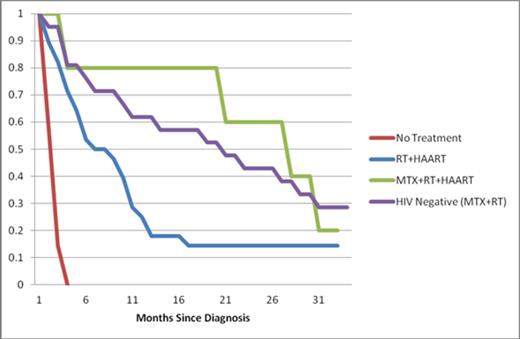
Parkland Memorial Hospital is a 950-bed acute care hospital located in Dallas, Texas. It serves as the county hospital for the city of Dallas as well as the primary teaching site of the University of Texas Southwestern Medical Center. After approval by the institutional review board, we identified patients with biopsy proven PCNSL between 1998 and 2012 at Parkland Memorial Hospital through the institution's tumor registry. After patient identification, the medical records were reviewed for the following patient data: age at diagnosis, ethnicity, sex, HIV status, CD4 cell count, HIV viral load, neuroimaging, treatment (radiation therapy and/or chemotherapy), date of death and date of last contact. Survival data and date of death were obtained from our tumor registry, chart reviews, and social security death index searches. Kaplan–Meier survival curves were constructed and compared between the two groups using the log rank test.
40 HIV-positive and 21 HIV-negative patients were included in this retrospective analysis. PCNSL was diagnosed by histological evaluation of biopsy specimens in all 61 patients. Patients were stratified based on their HIV status. Baseline demographic information for the two groups is compared in table 1. Median survival was 21.3 months and 4.6 months for the HIV-negative and HIV-positive cohorts respectively. All HIV-negative patients were treated with HD-MTX based regimens in addition to WBRT (MTX+RT). Of the HIV-positive patients: 28 received WBRT plus HAART (RT+HAART), 7 received no treatment and 5 received HD-MTX based regimens plus WBRT and HAART (MTX+RT+HAART). The average CD4 count at diagnosis in patients who did not receive treatment was 9.1, 50.6 in those who received RT+HAART and 155.8 in those who received MTX+RT+HAART although these differences did not meet statistical significance (p=0.056), (Table 2). HIV-positive patients who received RT+HAART had significantly better overall survival (OS) than those who received no treatment (p-value of log-rank test 0.00023) but worse OS than those who received MTX+RT+HAART (p= 0.0121). There was no difference in OS between HIV-positive patients who received MTX+RT+HAART and HIV-negative patients who received MTX+RT (p= 0.778), (figure 1).
Baseline patient demographics
| . | HIV-Positive (n = 40) . | HIV-Negative (n = 21) . |
|---|---|---|
| Age at Diagnosis (range) | 38.4 (24-52) | 53.3 (22-81) |
| Sex (male) | 32 (80 %) | 15 (71.4 %) |
| Ethnicity | ||
| White (non-hispanic) | 8 (20 %) | 8 (38.1 %) |
| Black | 21 (52.5 %) | 3 (14.3 %) |
| Hispanic | 11 (27.5 %) | 6 (28.6 %) |
| Asian | 0 (0 %) | 4 (19.0 %) |
| . | HIV-Positive (n = 40) . | HIV-Negative (n = 21) . |
|---|---|---|
| Age at Diagnosis (range) | 38.4 (24-52) | 53.3 (22-81) |
| Sex (male) | 32 (80 %) | 15 (71.4 %) |
| Ethnicity | ||
| White (non-hispanic) | 8 (20 %) | 8 (38.1 %) |
| Black | 21 (52.5 %) | 3 (14.3 %) |
| Hispanic | 11 (27.5 %) | 6 (28.6 %) |
| Asian | 0 (0 %) | 4 (19.0 %) |
HIV-positive patients stratified by treatment.
| . | No Treatment (n=7) . | WBRT+HAART (n=28) . | MTX+WBRT+HAART (n=5) . |
|---|---|---|---|
| Average CD4 Cell Count | 9.1 | 50.6 | 155.8 |
| Average Viral Load | 428,766 | 457,529 | 266,893 |
| Median Survival (Months) | 1.1 | 6.8 | 26.6 |
| . | No Treatment (n=7) . | WBRT+HAART (n=28) . | MTX+WBRT+HAART (n=5) . |
|---|---|---|---|
| Average CD4 Cell Count | 9.1 | 50.6 | 155.8 |
| Average Viral Load | 428,766 | 457,529 | 266,893 |
| Median Survival (Months) | 1.1 | 6.8 | 26.6 |
The data from our current study suggests HIV-positive patients with PCNSL can achieve similar overall survival as their HIV-negative counterparts when they receive similar chemotherapeutic regimens. Furthermore, RT+HAART appears to offer inferior OS to MTX+RT+HAART despite similar baseline CD4 counts.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal