Abstract
Follicular lymphoma (FL) is a disease with very heterogeneous course ranging from the indolent forms to rapidly progressive cases with poor outcome. Optimal therapy in FL patients with high tumor burden is immunochemotherapy (R-CHOP is the most frequent regimen used), followed by maintenance treatment. Data from randomized prospective studies (PRIMA) showed poorer outcome in those with high risk disease in terms of lower CR rate, higher risk of relapse and lower efficacy of maintenance therapy. Data comparing up-front intensive approach in younger fit patients and R-CHOP are limited.
To analyze long term results of intensive treatment protocol (R-sequential chemotherapy) in comparison with age, FLIPI and maintenance delivery matched (R-CHOP) controls.
Here we analyzed data of 48 prospectively enrolled FL patients who were treated by sequential (R-SQ) chemotherapy with or without up-front autologous stem cell transplant (ASCT) as a part of stratified risk adapted treatment in one institution. For R-SQ regimen were indicated patients<65 years with INT-FLIPI (with at least 2 additional risk factors: bulk and/or elevated B2M>3mg/L and/or thymidine kinase>15 IU/L) or HIGH-FLIPI patients (irrespective of additional risk factors). R-SQ protocol consists of alternating three cycles of etoposide-doxorubicine regimen (PACEBO), one methotrexate-ifosfamide regimen (IVAM), and one cycle of high dose cytarabine regimen (HAM). Remission was consolidated with 6th cycle of chemotherapy (PACEBO) in INT-FLIPI patients (n=22, 46%) or with ASCT with BEAM-200 conditioning (n=26, 54%) in HIGH-FLIPI patients. Maintenance immunotherapy was applied for historical reasons in 24 patients (50%). Controls were randomly selected from the Czech Lymphoma Study Group (CLSG) database from 626 cases with confirmed FL grade I to IIIa, treated with R-CHOP. Pair matching was performed on 1:3 basis, controls were matched by age, FLIPI and rituximab maintenance application. In the end, we analyzed intensive SQ-group (n=44) and standard control R-CHOP-group (n=144). Maintenance therapy was delivered to 24 patients (50%) in R-SQ group and to 72 patients (50%) in R-CHOP-group (P=1.00).
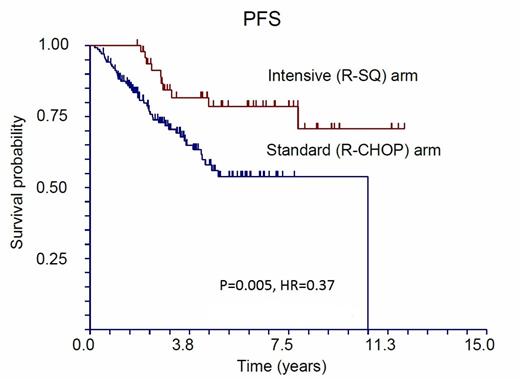
Median age of SQ-group was 47.6 years compared to 48.7 years in R-CHOP (P=0.44), FLIPI index was equally distributed: INT-FLIPI (43% vs 43%), HIGH-FLIPI (57% vs 57%, P=1.00). Treatment response quality was higher in SQ-group than in R-CHOP-group: CR/CRu 93.8% vs 70%, PR 6.2% vs 23% and SD/PD 0% vs 8% respectively (P=0.01). During the follow-up, (median 3.5 and 6.1 years in R-CHOP and SQ-group respectively, P<0.01) 10 patients (20.8%) relapsed or progressed in the R-SQ-group, and 41 (29%) in the R-CHOP-group (P=0.01). Only two of 48 patients (4.2%) died in the R-SQ-group, whereas twelve (8.7%) died in the R-CHOP-group (P=0.03). Five-year progression-free survival (PFS) was superior in the R-SQ-group with 78.5% (95% CI 0.66-0.91) survival compared to 53.8% (95% CI 0.43-0.65, P=0.005, HR=0.37) in the R-CHOP-group. Five-year overall survival (OS) was 100% in the R-SQ-group and 91.9% (95% CI 0.86-0.97, P=0.027, HR=0.18) in the R-CHOP group. When analyzing patients who received maintenance therapy, we found no difference in OS (P=0.13), but there was still significant difference in 5-year PFS in favor of the R-SQ-arm (88.4% and 58.2%, P=0.034).
In risky FL patients, intensive front-line therapy brings about 24% advantage in CR rate, about 25% higher 5-year PFS (reduces risk of relapse/progression by 62%) and about 10% advantage in 5-year OS (reduces risk of death by 82%). Maintenance immunotherapy application overshadows OS but not PFS advantage of intensive chemotherapy. Finally, in younger physically fit risky patients, more intensive induction regimen leads to superior disease control a remission duration compared to standard R-CHOP.
Supported by grants: LF-2013-004, IGA NT12193-5/2011 and PRVOUK-27/LF1/1. We would like to thank to all referring physicians: Jan Pirnos (Ceske Budejovice), Katerina Kubackova (FN Motol), Lucie Barsova (Liberec), Petr Kessler (Pelhrimov), Jitka Jakesova (Pribram), Milan Lysy (Usti n. Labem), Jindra Ciberova (Znojmo), Dagmar Adamova (Opava), Milan Matuska (Ostrava), Martin Brejcha (Novy Jicin).
Trneny:Roche: Honoraria, Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal